While there are many different mental health conditions and addictions that patients can struggle with, the Indiana Center for Recovery shared this insighted FAQ for two common ones: alcohol addiction and depression.
Shared with permission from our friends at the Indiana Center for Recovery
Is there a relationship between alcohol and depression?
Alcohol abuse is the root cause of many health issues. Depression is one example of this. People who binge drink are more prone to feel depressive signs—people with hangovers are at the most risk.
Consuming more than eight drinks in a single session for men or six for women is binge drinking. Aside from increasing your risk of accidents and injuries, it can also lead to other health issues, including alcohol poisoning.
Consult your doctor to know more about the relationship between alcohol and depression.
How does alcohol affect your mental health?
Alcohol is a depressant, which can alter your mood by disturbing your brain’s working. You may feel relaxation and reduced anxiety after drinking. It is because it impacts the area of your brain that regulates inhibition.
But, these results go away shortly. Your brain’s chemical changes may soon cause you to feel negative emotions. Alcohol slows down data processing in the brain. It makes it difficult to fix your true feelings.
Alcohol cuts the number of neurotransmitters in our brains. But, we need a specific amount to prevent anxiety. You would need to drink more to cope with these distressing emotions.
How long does alcohol-induced depression last?
The length of an alcohol-induced depressive episode varies from person to person. You may improve your signs if you don’t drink for a specific time. Some people may use other ways to get the same results. But, in most cases, the answer is usually 3–4 weeks.
Some research has shown that if the signs of depression persist after stopping drug or alcohol use, depression may take a severe form. Visiting a rehab center can help you in such a situation.
Can alcohol cause severe depression?
Alcohol is a depressant. If you drink frequently, it can start a depressive cycle. The majority of the time, binge drinking results from an underlying problem. As a result, you may develop clinical depression.
When you drink, you can make decisions you wouldn’t typically make. You’ll later come to regret, leading to despair. A cycle of depression might be triggered by simply realizing that you are not in control of yourself.
Alcohol hangovers can provide a highly depressed, ill, and depressing feeling.
“More than one in four adults living with serious mental health problems have a substance use problem,” according to the website MentalHealth.gov.
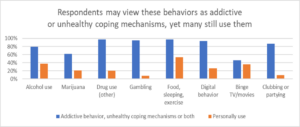
From restricted or binge eating to excessive gambling to extreme social media use, 77% of Americans surveyed say they have used at least one addictive behavior and/or unhealthy coping mechanism to manage their mental health issues, according to the GeneSight® Mental Health Monitor, a nationwide survey from Myriad Genetics, Inc. (NASDAQ: MYGN).
Though they may view these behaviors as addictive or as unhealthy coping mechanisms (or both), many admit to still using them.
“Mental health and addiction often go hand-in-hand,” said Morgan Freas, PharmD, a senior medical science liaison with Myriad Genetics. “Patients self-medicate with drugs, alcohol and destructive behaviors to help themselves feel better. Unfortunately, what they turned to for comfort ultimately causes more strife and struggle.”
According to the National Institute on Drug Abuse (NIDA):
“…substance use disorders often accompany other mental illnesses…For many people, drug and alcohol problems begin as self-medication: using substances to cope with temporary stress or to manage symptoms of chronic mental health problems they may not even know they have.”
“Fragmented and hard-to-access mental health care means that these conditions and addiction often go untreated. In some communities, it is easier to get illicit drugs than adequate medical mental health care, making co-occurring addiction and other mental illness more likely.”
The survey found those diagnosed with depression and/or anxiety consider drinking alcohol alone as an unhealthy coping mechanism, addictive behavior or both (77%). Yet, 41% of these respondents admitted to drinking alone to cope. In fact, 25% of this segment who said they heavily drank alone admitted they were worried they had a problem.
Treating addiction and mental health: a Psychiatric Nurse Practitioner’s (PNP’s) story
“Typically, people are trying to self-medicate an emptiness or a lack of something. And so it can look any different way, any way to get that dopamine response or that feel good response from any of the neurotransmitters that we get when we’re engaging in something that may or may not be healthy for us,” said Dawn Johnson, a psychiatric mental health nurse practitioner at the Indiana Center for Recovery.
Johnson studied to be a psychiatric nurse practitioner working in substance use disorder treatment after her husband died due to his addictions.
“So, my experience in self-medicating was with alcohol when I lost my husband to complications of his trauma and addiction and stress and pain,” said Johnson. “The only reason I’m here is because of my own journey with mental health and addiction and losing somebody so important to me to it. And what I tell my patients too is: I’m telling my late husband’s story to his children. Widows and widowers shouldn’t be telling the story. So that’s why mental health and addiction treatment is so important.”
Johnson shares her personal story when treating patients. She says that nearly all of the employees at the Indiana Center for Recovery have had previous addictions and mental health struggles, and that the employees will share their addiction history so that those in treatment don’t feel so alone.
“We just share this human experience. We try to normalize it and we normalize screwing up. We don’t try to mask it,” said Johnson. “My goal for working with patients is for them to be here to tell their story. And they need to be the hero in their own story. For so long, we were on the sidelines. We were the junkies being narcaned, and the EMTs were the heroes in our story. And it’s time for us to change the narrative. It’s time for us to rewrite our stories and be the hero.”
Medication trial and error may prompt unhealthy choices
The GeneSight Mental Health Monitor survey found that two-thirds of those diagnosed with depression and/or anxiety have experienced trial and error in trying to find medication that works for them. Nearly half of respondents (45%) report they have turned to an unhealthy coping mechanism as a result of a medication failure.
Those diagnosed with depression and/or anxiety admitted to using the following coping mechanisms:
- Sleeping too much or too little – 70%
- Withdrawing from social activities – 64%
- Binge watching TV or movies – 49%
- Skipping work/school/household responsibilities – 48%
To get them back on track, Johnson treats patients using a variety of mechanisms, including mental health medication treatment. Nearly all of her patients who come to the Center have tried and failed at least one mental health medication, which is extremely frustrating for the patient and can cause additional worry and reluctance to try new medication.
“When patients come to us, usually they’ve had multiple medication failures. Maybe they were on two or three medications, so multiple side effects – and they may have been taking medications to treat the side effects,” said Johnson. “So, they are feeling like they’re really not getting the relief that they need. And then a clinician will order something else or increase dosage … and that process starts over again. So, patients might feel numb to everything. They might feel anxious, and we find out it’s because one of the medications that they’re on is actually making things a little bit worse. They’ll come in feeling so hopeless, ‘Now I’ve got to start over again?’ And so, it’s just this repeat, repeat, repeat.”
To counter this, one of the first things she does is order a GeneSight test for those patients who have experienced mental health medication failure. GeneSight analyzes how a patient’s genes may affect their outcomes with medications commonly prescribed to treat depression, anxiety, ADHD, and other mental health conditions.
“Many of my patients have struggled with depression and/or anxiety, but failed to find a treatment that made them feel better. So, they resorted to alcohol, drugs or destructive behaviors to sooth themselves, as these offered short-term relief,” said Dawn Johnson, a psychiatric mental health nurse practitioner at the Indiana Center for Recovery in South Bend. “However, this behavior resulted in worsening mental health and destruction of their lives. I’ve seen it personally.”
“The GeneSight test has been very helpful with my patients because they can see that many of the medications that failed were in their moderate or significant gene-drug interaction categories. This means they may not have been metabolizing them properly, along with experiencing no symptom relief or horrible side effects,” said Johnson. “The GeneSight report reassures them that we’re not just throwing medications at them, we’re actually customizing their plan based on their genetic makeup.”
The survey found that of those who were told they have a problem, 58% of those diagnosed with depression and/or anxiety say mental health treatment helped relieve their addiction concerns.
The link between addiction and mental health
Nearly all surveyed Americans (94%) agree that substance and behavioral addictions often mask underlying mental health issues. Scientists and clinicians have long studied the link between addiction and mental health. While research is still ongoing, it is clear that mental health and addiction can – and do – occur together.
“Certain substances can cause people with an addiction to experience one or more symptoms of a mental health problem,” according to MentalHealth.gov. “Mental health problems can sometimes lead to alcohol or drug use, as some people with a mental health problem may misuse these substances as a form of self-medication.”
There is often the question of what comes first – mental health disorders or addiction. Unfortunately, there isn’t often a clear cause/effect.
However, childhood trauma may be an important factor leading to addiction. One study found that more than three in four (77%) of adult participants with substance use disorder (SUD) and post traumatic stress disorder (PTSD) had at least one childhood trauma before the age of 16, National Institute of Health (NIH).
According to an article in Verywell Mind
“…in many people with addictions, there is an underlying mental health issue as well. While neither condition actually causes the other, they do often exist together. What’s more, one condition can exacerbate the symptoms of the other. To better understand how comorbidity is possible, it helps to recognize that both are chronic brain disorders. In other words, when someone struggles with an addiction, their brain has been permanently rewired by the substance they abused. This, in turn, causes the brain to function differently than before. Just like diabetes or heart disease, a person with an addiction must manage their condition for the rest of their life. It is not as simple as stopping the drug use or alcohol condition. Many times, this is simply not possible.”
“Likewise, the changes that take place in the brain due to substance abuse occur in the same brain areas that are impacted by depression, anxiety, schizophrenia, and bipolar disorder. Consequently, it should not be surprising that there is a high rate of comorbidity between addiction and other mental illnesses. While the link is complex, some mental health issues increase the risk factors for substance abuse. What this means is that some people with mental illnesses will turn to alcohol or drugs to cope with the pain of their mental health issues.”
Jenna’s mental health journey
That was the case with Jenna, a former addict who is a year clean and now an employee of the Indiana Center for Recovery.

Jenna knew she needed help, when she was arrested and saw that she only weighed 79 pounds – about half her normal body weight. When she was in recovery, she realized she needed to not only detox and treat her addiction, but she also needed to work on her mental health.
Yet, many of the medications that Jenna had previously tried to help her anxiety and depression caused side effects that made her feel worse instead of better.
“I was taking antidepressants and anxiety medication, and I felt drowsy and I didn’t want to get out of bed because my stomach was upset. I was nauseous,” said Jenna. So, she was reluctant to try something else. “…waking up day in and day out, just feeling like you got hit by a bus, it takes a toll on you, especially when you’re in detox or in a facility trying to get better. And you can’t go to groups because you feel like garbage. You can’t interact with other clients because you feel like garbage.”
Johnson, who led Jenna’s treatment, ordered a GeneSight test.
“So, when I took the GeneSight test, I realized the previous medication just wasn’t as effective,” said Jenna. “Taking the GeneSight test really helped me. It is extremely beneficial for your mental and physical health.”
For more information about this topic and others, please read:
- Read more about the GeneSight Mental Health Monitor: https://genesight.com/mental-health-monitor/
- Watch Dawn Johnson and other addiction treatment clinicians talk about the link between addiction and mental health: https://genesight.com/genesight-cares/
- Join our Brighter Days Challenge: https://genesight.com/brighterdays/
While there are many different mental health conditions and addictions that patients can struggle with, the Indiana Center for Recovery shared this insighted FAQ for two common ones: alcohol addiction and depression.
Shared with permission from our friends at the Indiana Center for Recovery
Is there a relationship between alcohol and depression?
Alcohol abuse is the root cause of many health issues. Depression is one example of this. People who binge drink are more prone to feel depressive signs—people with hangovers are at the most risk.
Consuming more than eight drinks in a single session for men or six for women is binge drinking. Aside from increasing your risk of accidents and injuries, it can also lead to other health issues, including alcohol poisoning.
Consult your doctor to know more about the relationship between alcohol and depression.
How does alcohol affect your mental health?
Alcohol is a depressant, which can alter your mood by disturbing your brain’s working. You may feel relaxation and reduced anxiety after drinking. It is because it impacts the area of your brain that regulates inhibition.
But, these results go away shortly. Your brain’s chemical changes may soon cause you to feel negative emotions. Alcohol slows down data processing in the brain. It makes it difficult to fix your true feelings.
Alcohol cuts the number of neurotransmitters in our brains. But, we need a specific amount to prevent anxiety. You would need to drink more to cope with these distressing emotions.
How long does alcohol-induced depression last?
The length of an alcohol-induced depressive episode varies from person to person. You may improve your signs if you don’t drink for a specific time. Some people may use other ways to get the same results. But, in most cases, the answer is usually 3–4 weeks.
Some research has shown that if the signs of depression persist after stopping drug or alcohol use, depression may take a severe form. Visiting a rehab center can help you in such a situation.
Can alcohol cause severe depression?
Alcohol is a depressant. If you drink frequently, it can start a depressive cycle. The majority of the time, binge drinking results from an underlying problem. As a result, you may develop clinical depression.
When you drink, you can make decisions you wouldn’t typically make. You’ll later come to regret, leading to despair. A cycle of depression might be triggered by simply realizing that you are not in control of yourself.
Alcohol hangovers can provide a highly depressed, ill, and depressing feeling.