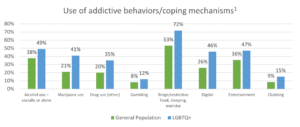
Nearly all (93%) LGBTQ+ respondents have turned to alcohol, drugs, binge or restrictive eating, gambling or other coping mechanisms to “deal with life’s problems,” according to the GeneSight® Mental Health Monitor, a nationwide survey from Myriad Genetics, Inc. (NASDAQ: MYGN). This is significantly higher than the general population, where 77% say they’ve used coping mechanisms or addictive behavior to cope.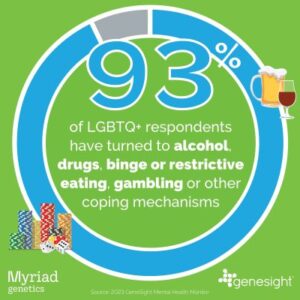
People who identify as lesbian, gay, bisexual, transgender, or questioning (LGBTQ) often face specific stresses and challenges that may increase their risk of behavioral health issues, according to the National Institute on Drug Abuse (NIDA) website. Additionally, data suggests that they may have higher rates of substance misuse and substance abuse disorders than people who identify as heterosexual.
“I have had suicidal ideation for decades, so I would try to find things [like coping mechanisms] to stop those thoughts even if just for a little bit,” said Rose, a transgender woman from Indiana. “The problem is these behaviors become unbalanced crutches.”
More than nine out of ten people who identify as LGBTQ+ agree that substance and behavioral addictions can mask underlying mental health issues.
Of those who turned to unhealthy coping mechanisms, 30% of LGBTQ+ survey respondents said turning to these coping mechanisms “helped” when they were dissatisfied with their mental health.
Finding an emotional escape
Some experts say LGBTQ+ community members may turn to substance use as a coping mechanism based on their past experiences, which often include trauma at a young age.
“In looking for acceptance, some LGBTQ+ community members may turn to dangerous behaviors to cope with the stress society places on them for being who they are,” said Dawn Johnson, a psychiatric mental health nurse practitioner with the Indiana Center for Recovery, who treated Rose.
“They’re vulnerable to feeling accepted, and so there’s certain behaviors or things they can get exposed to because someone will prey on them,” said Johnson. “We always have to be aware of what someone has been through. Has their family kicked them out and they’ve been vulnerable on the streets somewhere? How do we pull them back in and help them overcome some of these things that they’ve experienced when they’ve been put out without the support that they need?”
LGBTQ+ adults seek support, acceptance, and communication
The GeneSight Mental Health Monitor found that more than half of LGBTQ+ individuals surveyed agreed that talking to friends/family was the most helpful step in improving mental health symptoms if they were dissatisfied with their mental health in the past year. Nearly 40% agreed that “more support from family and friends” would be the most impactful step to improving their mental health in the future.
Johnson noted many individuals who are LGBTQ+ have experienced childhood trauma in the form of neglect and lack of acceptance.
 “LGBTQ+ individuals may have been treated poorly as a child and not learned what love is. Why? Because oftentimes the people who were responsible for teaching them about love looked at them with reproach, tried to change who they are, and judged them,” said Johnson. “So now as adults, LGBTQ+ individuals are in situations where we don’t know what love is really supposed to look like. And sometimes love can still be unhealthy, but yet it feels familiar, and it feels like it’s the right thing. But love isn’t supposed to hurt you and it isn’t supposed to be what’s best for someone else. So, learning to love the right way can be tough for LGBTQ+ adults, which may lead them to unhealthy coping mechanisms.”
“LGBTQ+ individuals may have been treated poorly as a child and not learned what love is. Why? Because oftentimes the people who were responsible for teaching them about love looked at them with reproach, tried to change who they are, and judged them,” said Johnson. “So now as adults, LGBTQ+ individuals are in situations where we don’t know what love is really supposed to look like. And sometimes love can still be unhealthy, but yet it feels familiar, and it feels like it’s the right thing. But love isn’t supposed to hurt you and it isn’t supposed to be what’s best for someone else. So, learning to love the right way can be tough for LGBTQ+ adults, which may lead them to unhealthy coping mechanisms.”
Stigma, discrimination, harassment can lead to mental health challenges
No two people’s experiences are the same. However, LGBTQ+ individuals continue to face social stigmas, discrimination, and an increased risk or harassment and violence, which may lead them to face more behavioral health challenges as a result, according to the NIDA website.
“Although the full range of [LGBTQ+] identities are not commonly included in large-scale studies of mental health, there is strong evidence from recent research that members of this community are at a higher risk for experiencing mental health conditions — especially depression and anxiety disorders,” according to the National Alliance on Mental Illness (NAMI) website.
“LGB adults are more than twice as likely as heterosexual adults to experience a mental health condition,” according to the NAMI website. “Transgender individuals are nearly four times as likely as cisgender individuals (people whose gender identity corresponds with their birth sex) individuals to experience a mental health condition.”
“LGBTQ+ teens may be two times as likely to be bullied, excluded or assaulted at school. And they’re nearly 40 percent less likely to have an adult in their family to whom they can turn. So it’s no surprise that they may be twice as likely to experiment with drugs and alcohol,” according to the Human Rights Campaign (HRC) website.
Disproportionate mental health challenges
The GeneSight Mental Health Monitor found that two out of three (66%) LGBTQ+ respondents said they were dissatisfied with their mental health in the past year – compared to only 46% of all adults surveyed.
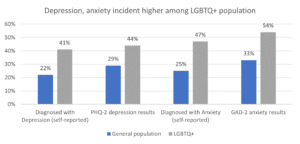
Nearly twice as many LGBTQ+ respondents say they are currently diagnosed with depression and/or anxiety than the general population (41% vs. 22% for depression, and 47% vs. 25% for anxiety).
On the positive side, the majority of this group (65%) indicate they have a trusted healthcare provider for their mental health needs, more than all adults surveyed (58%).
“Mental health can be very complicated, and especially for our trans population,” said Johnson. “Imagine having all the normal mental health issues that the population has in general, and then imagine being born in the wrong body and the struggles you might experience with that. It is a very precious population to work with. We want to help them love who they are, no matter what that might look like.”
Caring for the mental health of LGBTQ+ individuals
“My mental health was an invisible stone and it got heavy carrying it. By working on my mental health, I’m able to set down that stone and focus on engaging with the world,” said Rose. “The advice I would give other members of the LGBTQ+ community is that the first step to taking care of your mental health is finding a mental health professional. The second step is making sure that the clinician or therapist is right for you.”
According to Johnson, caring for a member of the LGBTQ+ community requires an understanding of what they’ve been through. Importantly, therapists and clinicians who create a safe environment with tenderness and compassion can help people feel empowered for the future, she said. She advises patients to look for a mental health professional who’s a good fit for the issues they need to address.
“Ask the right questions when you’re finding a therapist. Make sure and ask somebody, are you going to help me walk through this? Experience is a big part of it. A lot of the local organizations can give you a list of providers that can help with what you need specifically. So that way you’re not walking into setting where you might be treated ‘less than’ as you’re trying to figure out this whole journey that you’re on,” Johnson said.
Johnson tells patients to advocate for themselves throughout the process, including asking their clinicians for the GeneSight test to help inform their medication selection if their treatment plan includes mental health medication. GeneSight analyzes how a person’s genes may affect their outcomes with medications commonly prescribed to treat depression, anxiety, ADHD, and other mental health conditions.
Rose experienced trial and error with mental health medications for decades. Johnson ordered the GeneSight test for Rose.
“The GeneSight test didn’t take away my mental health struggles, but helped my clinician find a medication that made my issues manageable for the first time in my life,” said Rose. “I still have struggles, but having medication that helps me and minimizes my suicidal thoughts is huge. Having my depression and anxiety under control means that I have more time, ability and motivation to advocate for the LGBTQ+ community.”
In addition to provider recommendations from local LGBTQ+ organizations, a database of LGBTQ+ therapists is available through Psychology Today.
For more information about this topic, please visit:
- Seeking Better LGBTQ Mental Health
- Pride (and Prejudice) in LGBTQ+ Mental Health Treatment
- Why LGBTQ+ Mental Health is Important
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.