Could more fully integrated care models help ease current barriers to mental health treatment in the U.S? Advocates say yes.
As the number of Americans who do not receive needed mental health treatment continues to grow, poor access, high costs and poor outcomes for mental health treatment are often cited as reasons why. The latest Mental Health America (MHA) report notes that more than half (54.7%) of adults with a mental illness do not receive treatment. The report notes:
- “Millions of adults in the U.S. experience serious thoughts of suicide, with the highest rate among multiracial individuals. The percentage of adults reporting serious thoughts of suicide is 4.84%, totaling over 12.1 million individuals. 11% of adults who identified with two or more races reported serious thoughts of suicide in 2020 – 6% higher than the average among all adults.”
- “22.87% of adults who report experiencing 14 or more mentally unhealthy days each month were not able to see a doctor due to costs.”
- “In the U.S., there are an estimated 350 individuals for every one mental health provider.”
Advocates of integrated care say healthcare systems who are re-thinking how they combine behavioral and medical care services are showing that benefits may be possible for all involved.
What is an integrated care model?
“Integrated care is a general term for any attempt to fully or partially blend behavioral health services with general and/or specialty medical services. This blending can occur within inpatient or ambulatory clinical settings. By treating both the mental and physical needs of children, adolescents, and adults, we will better meet the triple aim of improved patient outcomes and satisfaction at a lower cost by addressing common, disabling and costly behavioral health problems (e.g., depression, anxiety, and substance use disorder),” according to the American Psychiatric Association (APA) website.
A video on the APA website shows how an integrated care model can be implemented in practice. It describes the research-backed Collaborative Care Model, in which psychiatric care services are delivered in a patient’s regular doctor’s office.
“Many patients with mental health and substance use concerns talk to their primary care providers or PCP first. PCPs traditionally have had two choices, treat the issue themselves or try to refer the patient to a mental health provider, like a psychiatrist … there simply aren’t enough providers to meet the need of all the referrals,” according to the video.
As the video continues, it shows how in the Collaborative Care Model, where a behavioral health care manager practices in the doctor’s office with the primary care team. They work with a consulting psychiatrist who keeps treatment on track and provides support for cases that need extra help. They use proven measures for assessment and treatment.
“It’s an organized approach that ensures patients receive the most effective care. And no one falls through the cracks. Treatment can include focused talking therapies and medication, when indicated, that’s prescribed by the PCP and overseen by the consulting psychiatrist. […] Collaborative care is happening right now all over the country and it’s reimbursable by insurance,” according to the video.
Is Integrated Care More Work Than the Regular Referral Process?
The current referral process isn’t foolproof. Managing out-of-network care referrals can be time-consuming and multiple referrals may be needed for a patient.
The integrated care model can make complex cases easier to manage and lead to improvement rates that can be more than doubled for common mental health conditions, such as Major Depressive Disorder, according to the APA website.
“PCPs are already managing mental illness and substance use disorders and are often frustrated with the extra work of collaborating with mental health clinicians outside of their typical referral network. They also express frustration with trying to keep up with evidence-based management of common conditions,” according to the APA’s website. “Quality integrated care programs substantially reduce the workload for PCPs through seamless communication and effortless expert consultation, vesting mental health outcomes solidly within a team-based framework that patients and clinicians alike can benefit from.”
How Does Health Insurance Work in Integrated Care?
The Centers for Medicare & Medicaid Services (CMS) and health insurance companies are working with many providers using integrated care models.
In the case of the Collaborative Care Model (CoCM), “The Centers for Medicare and Medicaid have announced billing codes for use by primary care providers to fund the Collaborative Care Model beginning in January 2017. Commercial payers around the country are now reimbursing for services delivered in CoCM – although, coverage and reimbursement varies by state, plan, and product,” according to the APA website.
Developing a more comprehensive approach
Pilot projects around the country are exploring how to enhance or expand integrated care strategies in various communities. The approach may be particularly valuable for specific patient populations.
“People with complex physical, behavioral health, and social needs often experience fragmented and ineffective care, leading to poor outcomes and high service use and cost,” according to the website for the Center for Health Care Strategies (CHCS), which is leading the Advancing Integrated Models project at eight pilot sites in the U.S.
“Each of these pilot sites will receive tailored, expert technical assistance, access to national subject matter experts, and participate in a peer learning collaborative to accelerate solutions across sites. CHCS will distill lessons and share best practices nationally to support other health care organizations seeking to adopt more integrated care models for individuals with complex needs,” according to the CHCS website.
As the conversation about integrated care continues, many are attempting to examine and improve upon current processes in order to better serve the needs of all involved. Rishi Manda, M.D., says on the CHCS website, “We need less of ‘do more’ and more of ‘do differently’ [in health care].”
For more information, please read these other articles on our website:
https://genesight.com/blog/healthcare-provider/the-value-of-thinking-through-a-communication-strategy-with-patients/
https://genesight.com/blog/healthcare-provider/pcps-are-you-playing-offense-or-defense-with-your-patients-mental-health/
https://genesight.com/blog/healthcare-provider/why-dont-some-common-antidepressants-work-for-patients/
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
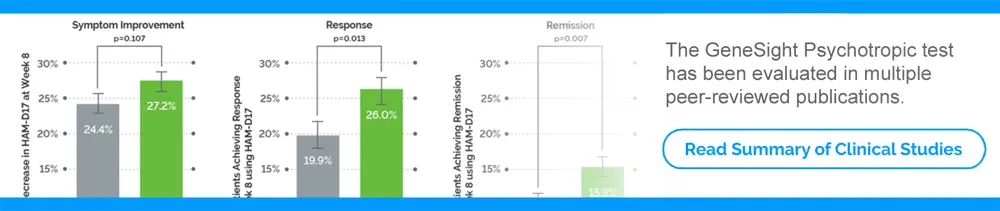
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.