If you are over 65, it makes sense to know the details of Medicare coverage. It is particularly important to take the time to clarify whether your plan covers the specific mental health services that you may need.
Why? The CDC estimated that 7 million of the nation’s 39 million adults aged 65 years and older were affected by depression.
Further, more seniors may be facing increased depression and anxiety due to loneliness as a result of the pandemic’s social distancing measures.
In 2020, more than 47.2 million people are Medicare Prescription Drug Plan beneficiaries, according to Centers for Medicare & Medicaid Services (CMS). If you are one of these millions, understanding the details of your plan is important, so you know what mental health services are covered by Medicare.
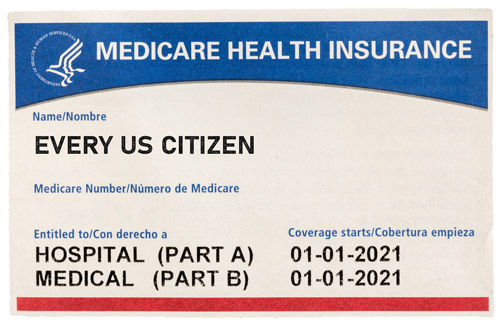
Medicare Health Coverage
In terms of overall healthcare coverage, Medicare covers a lot but not all costs, according to AARP. Plus, there are different coverage levels for Medicare depending on the plan you select.
“How much you pay for Medicare depends on which Medicare plan you choose; how often you go to the doctor or hospital; whether you have other health insurance; and whether you qualify for help with Medicare costs,” according to AARP.

“Medicare coverage is based on three main factors: federal and state laws; national coverage decisions made by Medicare about whether something is covered; and local coverage decisions made by companies in each state that process claims for Medicare,” writes Medicare on its website. “These companies decide whether something is medically necessary and should be covered in their area.”
Medicare advises patients to talk to their healthcare provider about whether Medicare will cover a specific service or supply. Medicare recipients can log into MyMedicare.gov or call 1-800-MEDICARE to answer specific billing questions and questions regarding claims, medical records, or expenses.
Does Medicare Pay for Mental Health Services?
While many find insurance policies to be complicated, understanding what mental health care services are covered by Medicare does not have to be an overwhelming experience.
There are many different types of Medicare plans: Original Medicare, Medicare Advantage, additional coverage through an employer plan. or Medigap Insurance.
What’s crucial – regardless of plan – is that before you reach out for specific guidance regarding your coverage and the subsequent costs, you should understand the basics of the benefits provided by Medicare Part A, Part B and Part D.
 Part A: Hospital Insurance
Part A: Hospital Insurance
Medicare Part A, or Hospital Insurance, helps pay for hospital care if certain conditions are met. This may include inpatient mental health services in either a general or psychiatric hospital, which could include:
- Semi-private rooms
- Meals
- General nursing
- Drugs as part of inpatient treatment
- Other hospital services and supplies
Part B: Medical Insurance
Medicare Part B, or Medical Insurance, helps cover mental health visits from a doctor and outpatient services. Coverage can include:
- One depression screening per year
- Individual and group psychotherapy
- Family counseling, if it helps with mental health treatment
- Certain lab and diagnostic testing
- Psychiatric evaluation
- Medication management
- Certain prescription drugs, like some injections
- Partial hospitalization
- Outpatient mental health services for treatment of alcohol and substance abuse
 Part D: Prescription Drug Coverage
Part D: Prescription Drug Coverage
Prescription Drug Coverage is part of the Medicare Part D plan and helps cover drugs that treat mental health conditions.
“Most Medicare drug plans have their own list of what drugs are covered, called a formulary. Plans include both brand-name prescription drugs and generic drug coverage,” writes Medicare in describing the coverage.
What does Medicare NOT Cover for Mental Health Services?
Medicare Part A Coverage does not include private-duty nursing, a phone or television in your room, personal items or a private room (unless medically necessary).
Medicare Part B Coverage does not include meals, transportation to/from mental healthcare facilities, certain activity therapies, certain support groups that are not group psychotherapy, and testing/training for job skills that are not a part of mental health treatment.
Medicare and Telehealth
In response to the COVID-19 pandemic, Medicare has temporarily expanded its coverage of telehealth services. These expanded, covered telehealth services will allow patients greater remote access to providers for services including common office visits, mental health counseling and preventive health screenings. This allows doctor visits from your home, reducing the risk of exposure to the virus.
Some added services include:
- Virtual check-ins, which are brief virtual services with a practitioner
- Online patient portals, which are a means to communicate with a practitioner without going to the doctor’s office
- Audio-only phone communications with practitioners if patient doesn’t have access to interactive audio-video technology
- Use of communication technology to have full doctor visits
While it is unclear whether Medicare will continue to add covered services as needs change in response to COVID-19 and its aftermath, some companies that provide mental health products and services are shifting the way they do business to accommodate the changes in the social and economic environment.
For example, as part of our COVID-19 response, we recently launched a new patient home collection kit for the GeneSight Psychotropic test. The kit, which still must be ordered by a licensed healthcare provider, allows DNA sample collection typically administered in a clinician’s office to be completed at home.
To learn more about how stay-at-home orders and social distancing are impacting healthcare, read this GeneSight post about telemedicine and telepsychiatry.
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.


 Part A: Hospital Insurance
Part A: Hospital Insurance Part D: Prescription Drug Coverage
Part D: Prescription Drug Coverage