Recent reports suggest more children are experiencing depression. In a study published in the Journal of Abnormal Psychology, rates of depression among adolescents aged 14 to 17 increased by more than 60 percent between 2009 and 2017.
“There is an overwhelming amount of data from many different sources, and it all points in the same direction: more mental health issues among American young people,” Jean Twenge, Ph.D., one of the study’s authors and a professor of psychology at San Diego State University, told Time Magazine. “There should no longer be any doubt. There is a mental health crisis among American teens and young adults.”

These numbers do not surprise Dr. Gene Beresin, executive director of The Clay Center for Young Healthy Minds at Massachusetts General Hospital and professor of psychiatry at Harvard Medical School. Dr. Beresin was quoted in the report saying: “We know that suicide and depression have been rising significantly. Kids are feeling more pressure to achieve, more pressure in school, and are more worried about making a living than in previous years.”
Now is the time to focus on childhood depression and other mental health illnesses. May 6 marks National Children’s Mental Health Awareness Day. According to the Substance Abuse and Mental Health Services Administration, this day shines “a national spotlight on the importance of caring for every child’s mental health and reinforces that positive mental health is essential to a child’s healthy development.”
Caring for a child’s mental health is a selfless task and a huge responsibility. Using pharmacogenomics in the pediatric population can make a difference and reduce trial and error in the prescribing process.
Prescribing Antidepressants in the Pediatric Population
Doctors often rely on several different factors in determining which medications may work for their patients, including:
- Patient experience
- Adverse effects
- Adherence
- Family history
- Cost
- Illness
However, two of these factors can be compromised when working with children.
First, pediatric patients may have difficulty articulating medication response; specifically, the efficacy of the medication and any side effects they may be experiencing. As a result, the “patient experience” portion of medication selection cannot be used if the patient cannot articulate his or her response.
Likewise, “adverse effects” can be compromised in the decision-making process. Prescribing medication for pediatric patients presents the potential for toxic or sub-therapeutic outcomes. This is because children experience changes in their metabolic activity, especially at a young age.
Pharmacogenomics Can Help Provide Insight
More doctors are starting to use pharmacogenomics in their practices to help guide medication decisions and overcome these challenges. Pharmacogenomics uses information about a person’s genetic makeup, or genome, to identify the drugs or drug doses that are likely to be genetically optimal for that patient.
The GeneSight Psychotropic test is one example of a pharmacogenomic test designed for use in mental health. Of importance to the pediatric population is pharmacokinetic information outlined in the GeneSight test results. These show genetic variation that may result in certain medications being broken down faster or slower than normal.
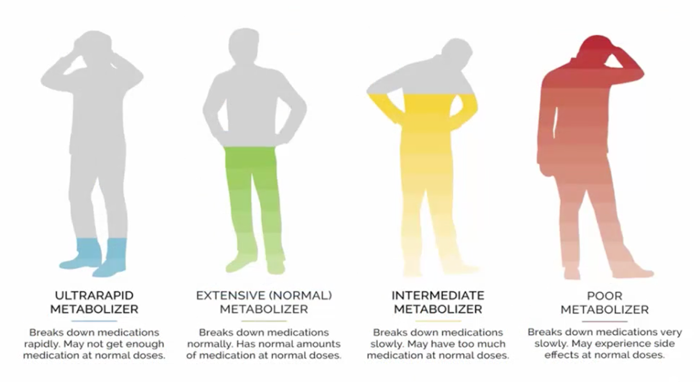
Pharmacokinetic genes can affect medication blood levels. There are four general types of metabolizers:
- An ultra rapid metabolizer breaks down medications rapidly and may not get enough of the medication at normal doses
- An extensive (normal) metabolizer breaks down medications normally and has normal amounts of medications at normal doses
- An intermediate metabolizer breaks down medications slowly and may have too much medications at normal doses
- A poor metabolizer breaks down medications very slowly and may experience side effects at normal doses.
Understanding How Physiological Changes Can Impact Pediatric Patients
Pediatric physiology can be very different from adult physiology. Enzymes responsible for breaking down medications will change based on a child’s age, but they will reach adult levels or above fairly early in life. Those enzymes that are not stabilized in childhood actually exceed adult levels before coming back down. For example, the hepatic enzyme CYP3A4 exceeds adult levels in childhood and then falls to normal adult levels at the end of puberty. The enzymes CYP2C9 and CYP2C19 exceed adult value at 3 to 4 years of age, but then decline to normal adult levels at the end of puberty. From a safety perspective, this is a good thing since it would likely result in the dosing being too low in children instead of too high.
Childhood and teenage depression can be challenging to treat, especially as more patients are presenting with these mental health issues. As your patients’ parents, guardians and caregivers share concerns about giving their child medication, pharmacogenomics can help alleviate some of the guess work when making decisions about dosage and which medications are genetically optimal for your pediatric patients.
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.