Trigger Warning: This webinar discusses suicide. If you or someone you know has suicidal thoughts, please call the National Suicide Prevention Lifeline at 988.
 |
W. Carson Felkel II, MD, FAPA – a psychiatrist and system medical director at Bon Secours Mercy Health in Greenville, S.C. |
 |
Debbie Thomas, EdD, APRN, PMHCNS-BC, PMHNP-BC, CMP – emeritus professor at University of Louisville School of Nursing; owner and medical director of Here & Now Psychiatric Services in Louisville, Ken. |
 |
Fay Bembry, FNP, PMHNP – psychiatric mental health nurse practitioner at Team Health in Johnson City, Tenn. |
*This blog summarizes key points discussed during Myriad Neuroscience’s fall 2021 Webinar:
Based on data collected by the Centers for Disease Control and Prevention (CDC), the American Foundation for Suicide Prevention (ASFP) reports that suicide is the tenth-leading cause of death in the United States. In 2019, more than 47,000 Americans died by suicide and there were an estimated 1.38 million suicide attempts according to the organization.
Conversations around suicide are often shrouded in misunderstanding and driven by fear. Cultural assumptions and misconceptions can heighten the stigma around suicide. Guilt, shame, and assigning blame may prevent honest conversations that can lead to healing.
What are the warning signs that someone might be thinking about suicide?
Recognizing the warning signs of suicide can start with knowing the unique ways a loved one tells a story, how they behave and/or how they express concern, said Dr. Felkel. He explained that actively listening for changes in how a person communicates may help identify cues that could indicate an escalation of emotion or intent to self-harm.

Dr. Thomas advised being aware of one’s own feelings along with those of their loved ones. Feeling like you are a burden to others, wanting to disappear, or sudden changes to your demeanor could signal that something is wrong, and help may be needed.
Some actions – like giving away items or changes in language – may also indicate that someone’s perspective on life has changed, according to Dr. Thomas.
Yet, Dr. Thomas and Bembry acknowledged that not everyone has a loved one who monitors them closely and sometimes the signs of distress are not obvious. This is why it’s so important for family members and friends to regularly check in on each other’s wellbeing.
“It really starts with asking someone how they’re doing and truly listening,” added Dr. Felkel. “If you don’t ask, sometimes they won’t tell you.”
When to reach out about suicidal thoughts
People should reach out for help any time they have suicidal thoughts, regardless of their intent to follow through on those thoughts, according to Dr. Thomas. “They don’t have to decide if it’s bad enough to reach out – they just reach out,” said Dr. Thomas, because those thoughts can escalate over time if left unaddressed.
Dr. Felkel noted that it can be typical for people to think about dying, especially while living in a “tough, broken” world.
“I think that this brokenness and this idea that pops into our heads that we wish we could die comes from feeling overwhelmed, like our resources do not match what we need to be successful,” said Dr. Felkel.
He explained that emergency care may be needed if a person struggles daily with suicidal thoughts and can’t escape those thoughts. Ideally, people can reach out to an outpatient therapist, outpatient psychiatrist, or primary care provider who can point a suicidal person to the right level of care.
Bembry often sees patients who have “better off dead” feelings, where older adults may have lost many of their loved ones and have chronic illnesses so they no longer want to live. She says these comments are common and even understandable among some geriatric patients who are in severe pain and can be separate and different from true suicidal ideation. However, Bembry says if these comments turn to talking about death, wanting death to happen, and trying to make death happen, that is different from only having “better off dead” feelings. In these situations, caregivers can ask their loved ones if they intend to harm themselves. If the answer concerns a caregiver, they should reach out to a trusted healthcare provider and explore treatment options.
Communication tips for conversations about suicide
As an adolescent and child psychiatrist, Dr. Felkel shared the advice that “the best thing parents can do is keep that open line of communication with your kids.”
While he admitted this can be easier said than done, being calm and unreactive while listening to children describe their challenges can help children trust their parents with their concerns. Having this open dialogue can give parents more opportunities to identify and recognize warning signs.
If an adolescent is going home after staying at an inpatient psychiatry unit, Dr. Felkel shared that it’s important that parents understand what is reasonable and realistic. While increased supervision is a common component of safety plans for when an adolescent returns home, constant supervision can be unrealistic and difficult for the patient and their caregiver.
Dr. Felkel also noted that it is important to take all mentions of suicide seriously, “and that when you do so, as you should, you also risk providing attention to a negative behavior, which rewards it. That’s not bad in and of itself, but it can create a cycle where kids will do negative behaviors, because unfortunately it gets their parents’ attention, and at the end of the day that’s really what kids want most, is for their loved ones to be with them.”
Instead, Dr. Felkel recommends sharing quality time, praise, and positive attention to encourage a healthier cycle of communication after a child reveals suicidal thoughts or attempts suicide. Dr. Thomas agreed, “Kids get hundreds of negative messages a day compared to a small number of positive messages. We take those for granted, but we land on all those negatives.”
For adults and older individuals, Bembry says it’s important to re-connect people with their purpose in life and the need for socialization, as social isolation may be one risk for suicide. “That’s probably one of the good things about social media or being able to connect socially with people on the Internet,” said Bembry.
Encouraging people to lean on their faith, church groups, re-connecting with family members, or having a pet are all ways Bembry recommended to help ground those with suicidal thoughts with their place in the world around them.
Likewise, Dr. Felkel said taking time to volunteer or serve others can help give people a purpose greater than themselves, fulfilling them by taking some focus off their struggles.
Safety planning for suicidal ideation
Each provider shared advice that may help suicide-attempt survivors, others struggling, and their loved ones identify and manage suicidal thoughts.
Bembry said an important first step is removing access to the means of suicide, which can help minimize the possibility that a person will attempt suicide amid a crisis.
Dr. Thomas creates individualized safety plans with her patients that shares resources, but also invites the patient to input the emergency contacts and steps they would take if they find themselves in a dark place.
“The best time to do safety planning is not during a crisis,” said Dr. Felkel, as people in crisis often don’t make the best decisions. Instead, it’s better to plan during periods of calm and to put those plans in writing.
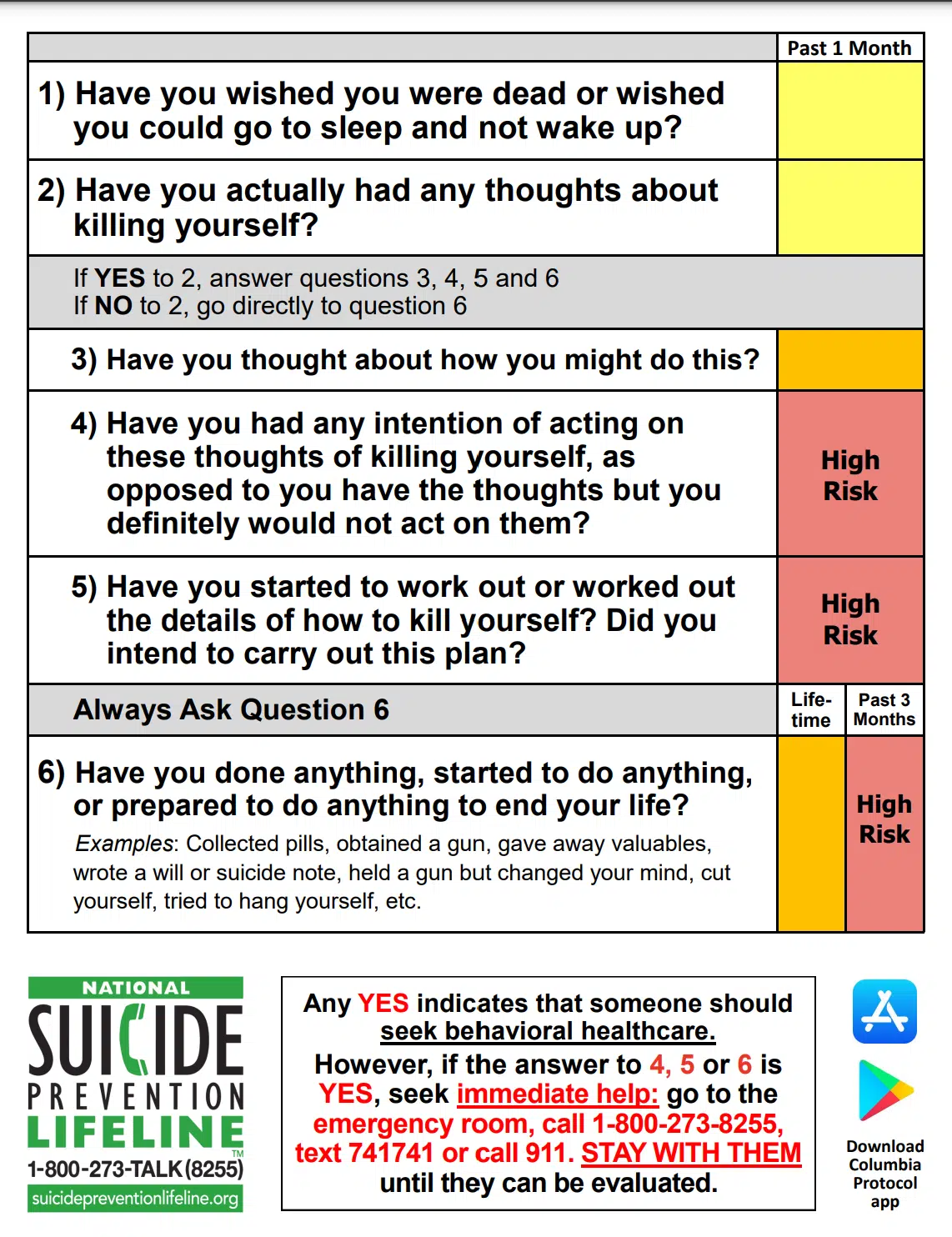
- Have you wished you were dead or wished you could go to sleep and not wake up?
- Have you actually had any thoughts about killing yourself?
- If YES to 2, ask questions 3, 4, 5 and 6
- If NO to 2, go directly to question 6
- Have you thought about how you might do this?
- Have you had any intention of acting on these thoughts of killing yourself, as opposed to you have the thoughts but you definitely would not act on them?
- Have you started to work out or worked out the details of how to kill yourself? Do you intend to carry out this plan?
- Have you done anything, started to do anything, or prepared to do anything to end your life?”
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
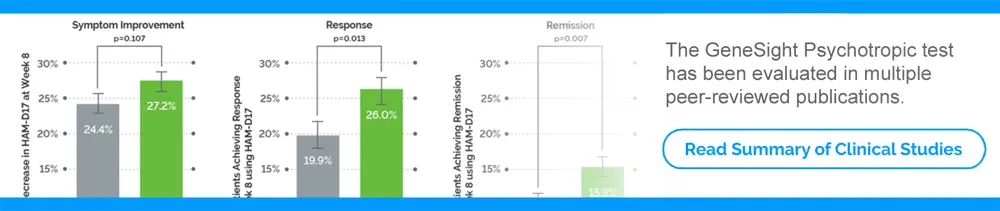
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.