Overview of Data Included in The GeneSight Algorithm
Evidence used to build the algorithm is derived from comprehensive literature and data reviews. Sources include published scientific literature (PubMed, Embase, Google Scholar, etc.), approved regulatory drug labels, and review applications (FDA). Animal-derived, preclinical data are excluded from assessment as only human based data are evaluated.
The data can be stratified into three categories:
- FDA reviewed pharmacokinetic (PK) and pharmacodynamic (PD) documents submitted as part of a new drug application (NDA).
- in-vitro (test tube) and in-vivo (human) data assessing medication pathways that have been published in peer-reviewed journals. This identifies the genes involved in the metabolism and/or the mechanism of action of a medication.
- in-vitro and in-vivo data evaluating genetic variations and applying expected activity levels (i.e. phenotype expression based on genetic variation) that have either been published in peer-reviewed journals or derived from internal lab data. This identifies to what extent the genetic variation is expected to impact the metabolism and/or the mechanism of action of a medication.
The quality of the data is scrutinized, with higher quality evidence having a greater impact in the algorithm. For example, in-vivo data will be held in higher regard than in-vitro data.
Additionally, data assessed by evidence grading bodies such as the Pharmacogenomics Knowledgebase (PharmGKB), and data evaluated by the Clinical Pharmacogenetics Implementation Consortium (CPIC) and the Dutch Pharmacogenetic Working Group (DPWG), are also evaluated for inclusion in order to ensure that all sources of clinically actionable gene-drug interactions (GDI) and genotype-phenotype relationships have been considered. However, our evaluation of the data may lead to different interpretations than what is concluded by individual expert PGx groups, evidence grading bodies, or other PGx companies..
The field of PGx is constantly evolving. As the evidence surrounding the impact of established and newly identified genetic variants on medication metabolism and response evolves, so too will the algorithm. Therefore, literature is collected and curated on a continuous basis. When enough new, quality literature has been accumulated for a particular gene-drug interaction, an internal committee determines if a change should be made. A full review of the GeneSight test is completed approximately every 1.5 – 2 years.
The GeneSight Algorithm: Stepwise Overview
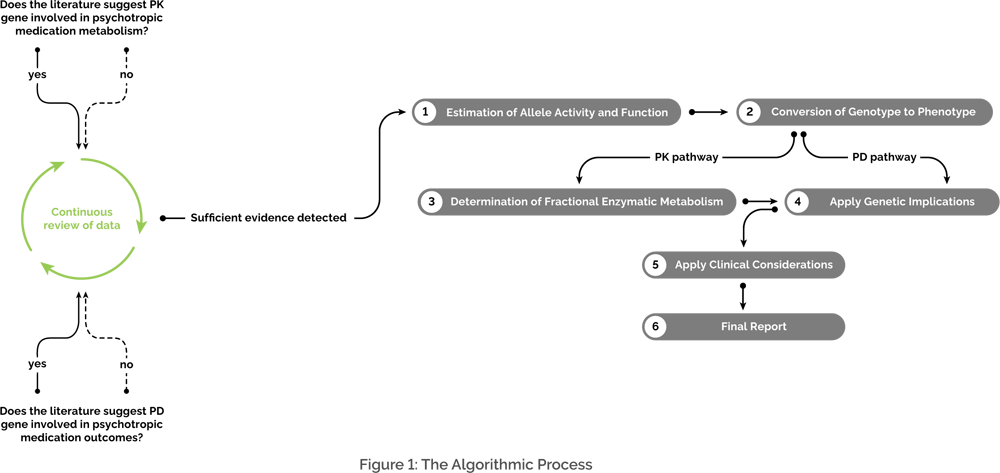
The algorithm can be broken down conceptually into the following steps. (Figure 1).
1: Estimation of Allele Activity and Function
An allele refers to different versions of a gene. Each allele that makes up a genotype is assigned an expected activity level or function. If the allele is pharmacokinetic (PK) in nature and codes for a phase 1 or phase 2 metabolic enzyme, then the *1 allele is used to designate the “wild type” allele, which is expected to have normal activity. For an allele to be assigned an activity level that is different than the normal *1 allele activity level, PK studies must have been conducted depicting variable activity for that allele. That “variant” would then be assigned either increased activity, reduced activity, or no activity..
If the allele is pharmacodynamic (PD) in nature, then consistent well-replicated findings from studies must have depicted that genetic variability is associated with variable outcomes, such as an increased risk of side effects or reduced response to a medication. PD allele genetic variability does not have standardized nomenclature like PK metabolic genes.
Please refer to our “Why doesn’t the GeneSight® test analyze certain genetic variants?” white paper for more information regarding criteria for adding a gene.
2: Conversion of Genotype to Phenotype
An individual’s combination of alleles for a specific gene is the genotype, while the effect of that specific combination is the phenotype.
For PK genes, the phenotype, or expressed enzyme activity level, depicts the metabolizer status and is assigned dependent on which alleles are detected. On the GeneSight test, the metabolizer status can be one of four phenotype groups (i.e., activity level groups): “extensive/normal”, “intermediate”, “poor”, or “ultrarapid”. The phenotype groups are determined by the expected total percent enzyme activity, which is calculated by adding together the percent enzyme activity of each individual allele. For example, an individual with *4/*5 for CYP2D6 would be categorized as “poor” considering that *4 and *5 alleles both result in no CYP2D6 enzyme activity. When total percent enzyme activity is calculated for this genotype, it is most consistent with the “poor” activity level. The percent enzyme activity levels are derived from the comprehensive literature and data review. These values, as well as metabolizer status ranges/cut-offs, are proprietary.
For PD genes, the phenotype would depict the likelihood of response or the risk of side effects and is dependent on which alleles are detected. On the GeneSight test, the likelihood of response would either be considered normal or reduced, and the risk of side effects would either be considered the standard risk or an elevated risk, depending on the respective PD gene and the genotype expressed. For example, an individual with the S allele for SLC6A4 would be expected to have a reduced response to certain SSRIs. It is important to note that not all medications evaluated will have PD implications.
3: Determination of Fractional Enzymatic Metabolism
To determine the percentage of enzyme involvement in the metabolism of a medication, a metabolic flowchart is internally constructed that is based on enzymatic pathway data. The flowcharts are comprehensive, and include
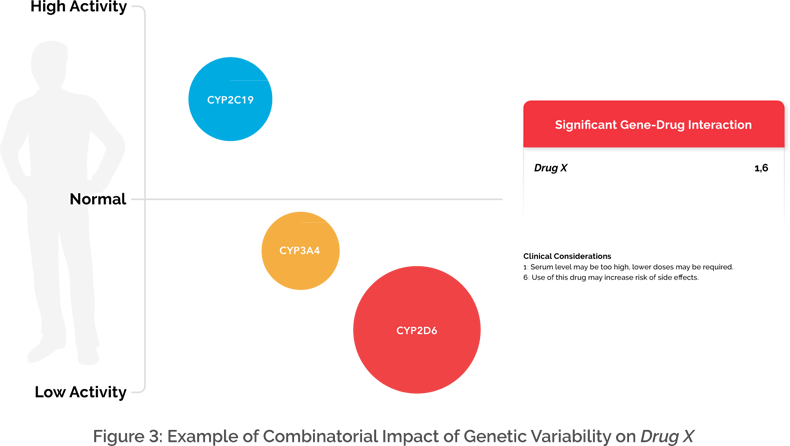
all potential metabolites, enzymatic pathways, and metabolic byproducts. The fractional involvement of enzymatic metabolism (i.e., the magnitude of enzyme involvement) is approximated based on the assessed literature. For example, let’s say for Drug X, evidence suggests that CYP2C19, CYP2D6, and CYP3A4 are involved in the metabolic process to variable degrees (Figure 2).
The assigned percentages (i.e., enzyme weight) are proprietary to the GeneSight algorithm. However, information regarding specific enzymatic involvement for each medication is depicted at the end of every GeneSight report in the Gene-Drug Interaction (GDI) chart. Once the weighted pathways are determined, an individual’s phenotype for each relevant gene can be applied to the algorithm. The algorithm is constructed with an assumption of normal metabolic phenotype activity (*1/*1). The actual genotypes that are run in the algorithm are changed to depict the individual’s detected phenotype (In the example listed above, the algorithm will be run with *4/*5 instead of *1/*1 for CYP2D6). Combinatorial phenotype weighting is proprietary for the GeneSight algorithm.
4: Apply Genetic Implications
To convey all potential outcomes and all possibilities, the algorithmic models are run using the relevant weights from the pathways involved and the individual’s phenotypes. To depict the algorithm, each enzyme involved in the metabolism of a medication is assigned a magnitude and direction. The magnitude is determined by how large of a role the enzyme plays in the overall metabolism of a medication. The direction is determined by the patient’s phenotype (i.e., whether increased or decreased activity is expected). Continuing with Drug X as our example, if the individual is a poor metabolizer for CYP2D6, an intermediate metabolizer for CYP3A4, and an ultrarapid metabolizer for CYP2C19, then the algorithm would depict the overall metabolism of Drug X to be reduced (Figure 3).
PD genetic considerations are also assessed to determine their potential impact on the likelihood of response or risk of side effects with certain medications. For example, the SLC6A4 gene has been shown in the literature to affect an individual’s response to the SSRI class of medications, specifically in the Caucasian population. If an individual carries the S allele of that gene, then the GeneSight algorithm would predict a reduced response to certain SSRIs. Both PD and PK genes play important roles in outcomes with medications. However, not all medications will be affected by both PD and PK genes. Based on a patient’s detected genetic variation, medications can either stay in the green “Use as Directed” category, or be placed into the yellow “Moderate Gene-Drug Interaction” or the red “Significant Gene-Drug Interaction” category.
5: Application of Clinical Considerations
Clinical considerations state the rationale for a medication’s classification and can help inform treatment decisions by providing information about how an individual’s genetic variation may impact outcomes. Please refer to our “How can I use the clinical considerations to help interpret the GeneSight® report?” white paper for more information.
6: Final Report
A report is generated that applies the previously discussed steps to all 64 medications screened. Based on the 14 genes evaluated in the algorithm, there are 995,328 possible combinations of phenotypes that an individual may have. The medications in each category of the report are listed in alphanumeric order, with medications with less clinical considerations being placed at the top of the list in alphabetical order, and medications with more clinical considerations being placed further down the list. Medication placement in each of the three categories is based on detected genetic variability and severity of GDI. Medication failure may still occur with medications in the “Use as Directed” category, and medications in the “Significant GDI” category may be effective, as all medications have unique efficacy and side effect profiles. PGx testing is intended to provide insight on how an individual’s genetic variation may affect outcomes with certain medications and should be used in conjunction with other clinical factors, expertise, and judgment. Therefore, PGx tests are intended to be ordered by and used only in consultation with a healthcare provider who can prescribe medications. The GeneSight test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of an individual’s medical history, other medications they may be taking, their family history, and other factors.
Conclusion
Most medications are processed via multiple metabolic pathways, with genomic variability being capable of influencing the rate of metabolism as well as the potential response or risk of side effects. Depending on the genomic variability, minor pathways when considered collectively may be more influential than a major metabolic pathway on metabolism. The GeneSight Psychotropic test uses a combinatorial approach that measures multiple genomic variants for each individual and weighs them in combination to provide comprehensive information about how an individual’s genetic variation may impact their outcomes with certain medications. The clinical validity and clinical utility of the GeneSight Psychotropic test have been evaluated in multiple published, peer-reviewed clinical trials.2-6
References
- Bousman CA, Eyre HA. “Black box” pharmacogenetic decision-support tools in psychiatry. Braz J Psychiatry. 2020;42(2):113-115. doi: 10.1590/1516-4446-2019-0724
- Hall-Flavin DK, Winner JG, Allen JD, et al. Using a pharmacogenomic algorithm to guide the treatment of depression. Transl Psychiatry. 2012;2(10):e172. doi:10.1038/tp.2012.99
- Winner J, Allen JD, Altar CA, Spahic-Mihajlovic A. Psychiatric pharmacogenomics predicts health resource utilization of outpatients with anxiety and depression. Transl Psychiatry. 2013;3(3):e242. doi: 10.1038/tp.2013.2
- Hall-Flavin DK, Winner JG, Allen JD, et al. Utility of integrated pharmacogenomic testing to support the treatment of major depressive disorder in a psychiatric outpatient setting. Pharmacogenet Genomics. 2013;23(10):535-548. doi: 10.1097/FPC.0b013e3283649b9a
- Tanner JA, Davies PE, Voudouris NC, et al. Combinatorial pharmacogenomics and improved patient outcomes in depression: treatment by primary care physicians or psychiatrists. J Psychiatr Res. 2018; 104: 157-162. doi: 10.1016/j.biopsych.2012.10.030
- Greden JF, Parikh SV, Rothschild AJ, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: a large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019; 111:59-67. doi: 10.1016/j.psychires.2019.01.003