Depression isn’t considered a normal part of aging. Older adults may, however, be at an increased risk of developing the condition — and diagnosing it can come with a specific set of challenges.
“The good news is that the majority of older adults are not depressed. Some estimates of major depression in older people living in the community range from less than 1% to about 5% but rise to 13.5% in those who require home healthcare and to 11.5% in older hospitalized patients,” according to the Centers for Disease Control and Prevention (CDC) website.
But depression is different for seniors in many ways. “Older adults are often misdiagnosed and undertreated. Healthcare providers may mistake an older adult’s symptoms of depression as just a natural reaction to illness or the life changes that may occur as we age, and therefore not see the depression as something to be treated,” according to the website.
One reason why diagnosing depression in geriatric patients is challenging may be that the symptoms can be different for their age group than for their younger counterparts. Somatic, or physical symptoms of depression common in younger people – such as weight loss, sleep disturbances and pessimism about the future – may occur in patients aged 65 years or older, but do not necessarily signal major depressive disorder, according to a study published in Aging & Mental Health.
A tool that is intended to help clinicians more accurately assess depression in older adult patients is the Geriatric Depression Scale (GDS). It can be the first step toward assessing depression in elderly patients.
What is the Geriatric Depression Scale?
According to the American Psychological Association (APA), the GDS “is a self-reported measure of depression in older adults.” The GDS considers the differences between how symptoms present in younger and older adults.
Developed by Dr. Jerome Yesavage and colleagues in 1983, the GDS uses a “yes/no” question format to screen for depression among older people. It was developed because previously administered questionnaires asked too many questions that overlapped with common aging disturbances. It uses a different approach than other depression screening tools.
 The GDS was originally created as a 30-item questionnaire. Since this version proved both time-consuming and difficult for some patients to complete, a 15-item version was developed.
The GDS was originally created as a 30-item questionnaire. Since this version proved both time-consuming and difficult for some patients to complete, a 15-item version was developed.
“The shortened form (GDS-S) comprised of 15 items chosen from the Geriatric Depression Scale-Long Form (GDS-L). These 15 items were chosen because of their high correlation with depressive symptoms […],” according to the APA article. “Of the 15 items, 10 indicate the presence of depression when answered positively while the other five are indicative of depression when answered negatively.” This shorter form is ideal for people who tire easily or have trouble concentrating for longer periods of time.
Some topics in the questionnaire include:
- Mood: “Do you feel happy most of the time?” or “Do you often feel helpless?”
- Participation in activities: “Have you dropped many of your activities and interests?”
- Outlook on quality of life: “Do you feel that your situation is hopeless?” or “Do you think that most people are better off than you are?”
- Concern about cognitive abilities: “Do you feel that you have more problems with memory than most?”
According to an article published in the International Journal of Geriatric Psychiatry, the GDS proved useful as a screening tool for both minor and major depression in older adults living in nursing homes with no cognitive impairment as well as with those with mild to moderate cognitive impairment.
Is the Geriatric Depression Scale reliable?
In a review of 53 studies published in the Archives of Gerontology and Geriatrics Journal, the GDS was found to be “highly useful for detecting depression among elderly with high sensitivity and specificity.” The studies included 17,018 participants.
The authors concluded that all forms of the GDS were able to detect both the presence of depression (sensitivity) and non-presence of depression (specificity).
According to the journal, “GDS 15 had pooled sensitivity and specificity of 86% and 79% with higher diagnostic accuracy (AUC = 0.90). GDS 10 had pooled sensitivity and specificity of 87% and 75% with AUC = 0.83. Our study found GDS 4 to have sensitivity of 74% with specificity of 71%.”
How is geriatric depression diagnosed?
Healthcare providers may use the Geriatric Depression Scale to assess late-life depression. They may use other screening tools, discussed in another GeneSight® blog post.

An older person can go to their primary care provider, rather than a specialist, for help with their symptoms or seek treatment from a mental health professional.
According to an article published in the Psychiatric Clinics of North America journal, “Many older adults prefer to receive their depression treatment in primary care, where providers can address not only mental health problems but also acute and chronic medical conditions that are common in this age group and often comorbid with depression. Primary care providers who provide continuity of care also have an important opportunity to track depression over time because depression in older adults is often chronic or recurrent. A number of research studies over the past 10 years have demonstrated that geriatric depression can be treated effectively when mental health providers effectively partner with their colleagues in primary care to provide effective consultation and collaborative care.”
How to access and administer the Geriatric Depression Scale
The GDS is available in the public domain, free to use, and is easy to administer and score.
The Stanford University Aging Clinical Research Center (where GDS developer Dr. Jerome Yesavage is a director), maintains a webpage which provides access to the short- and long-form original English language versions of the GDS. It includes versions of the scale in more than 30 different languages and provides information about scoring, basic references and mobile applications.
It usually takes between five to seven minutes to administer the 15-question test, according to a video published on the American Journal of Nursing website. In scoring the GDS, the healthcare provider gives one point for each answer that indicates depression. If a person scores greater than five on the 15-question assessment, it may indicate the presence of depression and help clinicians decide whether further assessment is needed.
“Positive response to these questionnaires should alert the primary care provider to further evaluate the patient for depression,” according to the Psychiatric Clinics of North America journal article. “Not all depressed patients will answer positively to these questionnaires, and to address the possibility of ‘false negatives,’ clinicians may wish to ask additional questions about depressive symptoms for patients who appear depressed, who have a difficulty engaging in care, or whose functional impairment seems inconsistent with objective medical illness.”
What are the risk factors and protective factors for geriatric depression?
The health conditions many people face as they get older may put them at a higher risk of developing depression overall compared to their younger counterparts, according to the CDC website.
“Older adults are at increased risk. We know that about 80% of older adults have at least one chronic health condition, and 50% have two or more. Depression is more common in people who also have other illnesses (such as heart disease or cancer) or whose function becomes limited,” according to the website.
According to the National Institute on Aging (NIA) website, there are also additional risk factors for depression in older adults. While these factors may not cause depression, research has shown that they may be related to the risk of a person developing it:
- “Medical conditions, such as stroke or cancer
- Genes – people who have a family history of depression may be at higher risk
- Stress, including caregiver stress
- Sleep problems
- Social isolation and loneliness
- Lack of exercise or physical activity
- Addiction and/or alcoholism
- Functional limitation that make engaging in activities of daily living difficult
- Addiction and/or alcoholism- included in Substance-Induced Depressive Disorder”
Although researchers continue to study these correlations, these factors may in some cases be related to changes people experience as they age.
“Everyone needs social connections to survive and thrive. But as people age, they often find themselves spending more time alone. Studies show that loneliness and social isolation are associated with higher rates of depression,” according to the website.
There are several factors that can help ward off or prevent geriatric depression, or situations or conditions that could offer long-term mental health benefits.
“Protective factors include social support and social activities such as volunteering and physical activity,” according to the Psychiatric Clinics of North America journal article. “Religion and spirituality may play an important part in many older adults’ lives. They may allow older adults to experience life as meaningful despite losses and challenges and, thereby, reduce the risk of depression. It is also possible that the positive effect of religion on mental health is mediated by the social connectedness and the social support derived from taking part in religious and associated social activities.”
While some cases of depression can’t be prevented, the following are steps older adults can take that may help, according to the NIA website:
- “Be physically active and eat a healthy, balanced diet. This may help avoid illnesses that can bring on disability or depression. Some diets — including the low-sodium DASH diet — have been shown to reduce risk of depression.
- Get 7-9 hours of sleep each night.
- Stay in touch with friends and family.
- Participate in activities you enjoy.
- Let friends, family, and your physician know when you’re experiencing symptoms of depression.”
What are the symptoms of geriatric depression?
Depression might look different in older people than in younger people, according to the NIA website. For some depressed older adults, sadness is not their main symptom. Instead, they could feel numb or have a lack interest in activities. They also may not be as willing to talk about their feelings.
According to an AARP article, “Sadness is a symptom we’re all familiar with, but depression symptoms aren’t limited to the mind. ‘In older people, depression tends to manifest itself more often with physical symptomology than in younger people. ‘I hurt more. I just don’t feel right physically,’ says Bruce Sutor, M.D., a psychiatrist at the Mayo Clinic, in Rochester, Minnesota. ‘Common symptoms: headaches, joint pain, fatigue, sleep disturbances, loss of appetite and gastrointestinal issues.’”
Some families may also notice a change in behavior in their older relatives, according to the article.
“Unfortunately, the disorder often goes untreated in older adults, in part because their depression can be challenging to diagnose. Their symptoms are often different than those of younger adults, says Ipsit Vahia, M.D., medical director, geriatric psychiatry outpatient programs, at McLean Hospital in Belmont, Massachusetts, and assistant professor of psychiatry at Harvard Medical School. Rather than the ‘classic’ symptoms of sadness, fearfulness or hopelessness, they tend to display symptoms such as irritability, a lack of motivation or energy, or a disruption in sleep patterns or appetite. ‘There’s also a tendency to start withdrawing,’ says John F. Greden, M.D., founder and executive director of the University of Michigan Comprehensive Depression Center. ‘That’s what families notice first.’ Many older adults – and even many clinicians – don’t recognize these symptoms as depression, especially because they often overlap with symptoms of other health conditions. Depression and dementia are especially easy to confuse, says Vahia.”
Below is a list from the NIA website of common depression symptoms. However, since people experience depression differently, this may not be a complete list.
- “Persistent sad, anxious, or ‘empty’ mood
- Feelings of hopelessness, guilt, worthlessness, or helplessness
- Irritability, restlessness, or having trouble sitting still
- Loss of interest in once pleasurable activities, including sex
- Decreased energy or fatigue
- Moving or talking more slowly
- Difficulty concentrating, remembering, or making decisions
- Difficulty sleeping, waking up too early in the morning, or oversleeping
- Eating more or less than usual, usually with unplanned weight gain or loss
- Thoughts of death or suicide, or suicide attempts”
Based on a person’s specific symptoms, they may be diagnosed with different forms of depression, according to the NIA website. The following are examples of different types of depression:
- “Major Depressive Disorder – includes symptoms lasting at least two weeks that interfere with a person’s ability to perform daily tasks
- Persistent Depressive Disorder (Dysthymia) – a depressed mood that lasts more than two years, but the person may still be able to perform daily tasks, unlike someone with Major Depressive Disorder
- Substance/Medication-Induced Depressive Disorder – depression related to the use of substances, like alcohol or pain medication
- Depressive Disorder Due to A Medical Condition – depression related to a separate illness, like heart disease or multiple sclerosis.
Other forms of depression include psychotic depression, postmenopausal depression, and seasonal affective disorder,” according to the website.
The unique challenges of diagnosing, treating and managing late-life depression
In addition to challenges in diagnosing late-life depression, there may also be obstacles in treating and managing the condition.
“Depression in older adults is more severe, lasts longer and has lower remission rates than in younger people, according to a recent study of adults ages 18 to 88 in the Netherlands,” according to an AARP article.
“Researchers there over the course of two years studied 1,042 adults diagnosed with major depression. They followed whether each study participant was still depressed after the two years, the severity of the depressive symptoms, the likelihood of experiencing remission and the degree of improvement in depression severity. The team found the outcomes for all four indicators worsened with age, especially for people age 70 and older,” according to the article.
Older adults in certain groups may face further challenges. Older women are at a higher risk than men of developing depression, according to the AARP article. Additionally, according to the Psychiatric Clinics of North America journal article:
“Older adults from certain ethnic/racial minority groups have higher rates of depression and are less likely to [be] diagnosed with or treated for depression than their white counterparts. These health service disparities in minority populations become increasingly complicated when considering cultural beliefs and practices of health and attitudes to depression care. Culture influences how individuals experience and express depression. Minority patients from certain ethnic groups may express their depression more somatically than psychologically. Such somatic presentations may reduce the recognition of depression by primary care providers or leads to the perception of a patient as ‘difficult.’ Some minorities may also have less faith in the biological etiology of depression, be more skeptical about antidepressant medications, and show stronger preferences for counseling than their White counterparts. When pharmaceutical treatment is the only available option, minority patients may be less likely to engage in treatment and more likely to be non-adherent. Our present primary care systems that focus primarily on pharmacological treatment without considering the unique barriers faced by ethnic and racial minority populations may not be effective in addressing the pattern of disparities observed.”
How is geriatric depression treated?
While a variety of factors may make it difficult for older adults to access or complete treatment, for most people, depression does get better with treatment, according to the NIA website.
Common forms of treatment for depression in older patients are not wholly dissimilar from those used in younger populations, for whom a combination of psychotherapy and medication are often prescribed. The American Psychological Association (APA) Clinical Practice Guidelines recommends three forms of psychotherapy along with a second-generation antidepressant, according to its website.
Recommended therapies include:
“Group Cognitive-Behavioral Therapy (Group-CBT)
Cognitive-behavioral therapy targets current problems and symptoms and focuses on the relationship among behaviors, thoughts, and feelings, and aims to change those patterns that reduce pleasure and interfere with a person’s ability to function at their best.
Interpersonal Psychotherapy (IPT)
Interpersonal psychotherapy focuses on improving problematic relationships and circumstances that are most closely linked to the current depressive episode. If considering this treatment for older adults with depression, the panel recommends augmenting with a second-generation antidepressant.
Group Life-Review/Reminiscence Therapy
Group life-review/reminiscence therapy helps older persons focus on their life arc, reviewing and reflecting on transitions and challenges, to arrive at a more balanced and accepting perspective of life.
Medications
Second-generation antidepressants (SSRIs, SNRIs or NDRIs) are recommended for older adults due to the reduced risk of side effects and safety in the event of overdose. If considering medication for older adults with depression, the panel recommends combining it with interpersonal psychotherapy.”
Considerations for antidepressants for geriatric depression
Some clinicians may recommend medication as part of a treatment program. There are some additional considerations may need to be accounted for when prescribing antidepressants to older adults compared to younger patients, according to an article in the American Family Physician. Many older adults take multiple medications for different conditions (known as polypharmacy), which puts them at greater risk for potential drug-drug interactions and adverse drug reactions.
While antidepressants have shown to be an effective treatment in managing depression, it can take trial-and-error to find one that’s effective for a particular individual. According to the AARP article:
“‘For managing major depressive disorder, antidepressants in combination with psychotherapy seem to work more effectively than either form of treatment by itself,’ says Vahia. In a 2020 review of several studies on antidepressant success rates, the NIH reported that when patients are treated without antidepressants, about 20 to 40 out of 100 people who took a placebo saw their symptoms improve within six to eight weeks. For those treated with antidepressants, about 40 to 60 out of 100 people noticed an improvement in the same time period. Prescribing antidepressants isn’t a precise science. Similar to treating high blood pressure, it takes time to figure out the right medication. ‘About 35 percent of people will respond to the first antidepressant they’re put on,’ says Maria A. Oquendo, M.D., chair of psychiatry at University of Pennsylvania’s Perelman School of Medicine and president of the American Foundation for Suicide Prevention. ‘By the third trial, about 65 percent will respond.’”
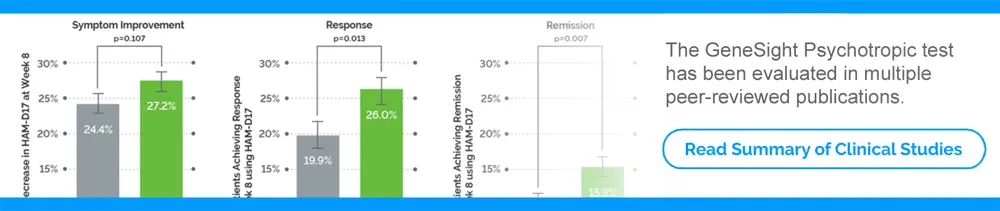
As a result, a clinician may consider genetic testing to help inform medication selection and dosing. The GeneSight test is a pharmacogenomic test that evaluates clinically important genetic variations in a person’s DNA. The results of the GeneSight test can inform the clinician about genes that may impact how an individual metabolizes or responds to medications commonly prescribed to treat depression, anxiety, ADHD and other psychiatric conditions.
Additional support for geriatric depression patients
In addition to psychotherapy and medication, social support may make a difference in a person’s depression treatment, according to the Psychiatric Clinics of North America journal article.
“Family members often play an important role in patients’ treatment engagement and adherence. Up to half of depressed older adults fail to take a significant proportion of prescribed antidepressant medication, and recent research indicates that perceived emotional support from family and friends is a critical predictor of adherence. In clinical practice, a provider’s explicit, expressive, and constant message of commitment to the patient’s improvement is an important step to engaging the patient and to increasing his or her adherence to treatment,” according to the article.
For more information about this and other topics, please visit:
How to Recognize Depression Symptoms in Seniors
Helping a Senior Loved One with Depression: A Caregiver’s Guide
Carlo Bayrakdarian, MD, geriatric psychiatrist healthcare provider story
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.