*This blog summarizes key points discussed during the May 2023 GeneSight® Cares webinar
Participants:



Most Americans acknowledge a connection between unhealthy coping mechanisms and a mental health condition like depression or anxiety, according to the Spring 2023 GeneSight Mental Health Monitor. Some unhealthy coping mechanisms respondents acknowledged as problematic included excessive sports gambling, binge watching TV/movies, over or under sleeping or eating, and extreme video gaming.
A group of experts discussed in a recent GeneSight Cares webinar how important it is to dissuade patients from engaging in these unhealthy behaviors and treat possible underlying mental health issues.
Hundreds of participants heard from our panelists about unhealthy coping mechanisms, how to bring the conversation to the potential underlying mental health issue, and how the GeneSight test may provide more information to clinicians to aid in a patient’s treatment.
Increasing drug use and unhealthy coping mechanisms
Dr. Lisa Marie Reyes-Walsh, a psychiatric nurse practitioner and educator in Woodstock, Ga. said she sees “a myriad of unhealthy behaviors. From cell phones, social media, eating behaviors, eating disordered behaviors (either overeating or under eating), and then more recently, pornography (having an issue with pornography with social media). So that’s been a big, big issue I’ve seen lately.”
Some of the behaviors identified in the Spring 2023 GeneSight Mental Health Monitor included:
- Alcohol use – Socially or alone
- Marijuana – Smoking or edibles
- Drug use – Sedatives, stimulants, hallucinogens, anesthetics, or inhalants (not including marijuana)
- Excessive gambling – Sports or non-sports
- Binge/restrictive food, sleeping, or exercise
- Excessive social media or video gaming
- Binging TV or movies
- Clubbing/partying
“We see a huge increase – in our teenagers, adolescent and college students, and a lot of the young professional adults as well – drastic increase with drugs, alcohol and what I refer to as ‘gas station drugs.’ In Mississippi, we have a lot of things that are sold over the counter, that are sort of outside of the purview of being legally restricted,” said Dr. Stephen Pannel, a psychiatrist, DO, ABPN, ABAM and chief medical officer, Right Track Medical Group in Oxford, Miss. “So, we just have seen a huge increase with that. A lot of vaping, you know, a lot of these different things that are out there now can be vaped and used in vape cartridges. So, ours by far and away is more of … chemical use increase than anything else we’re seeing.”
How COVID has changed the addiction landscape
The COVID pandemic had a significant impact on patient care – and on those with addiction and mental health issues. Dawn Johnson explained:

“Once COVID hit, our facility went from probably 40 patients to about 140 in about three months because other places were shutting down and people were dying. I had patients who were dying because they went home and they were drinking, they were working from home. And of course, everything’s accessible.”
“I think there [are] a lot of people with trauma. Whether it is trauma they realized they had, and this isolation also triggered a childhood trauma response, or if they just, you know, going through the pandemic, they’ve experienced trauma and fear, that is that basis.”
“I get these 18- and 19-year-old kids and their important years in high school were affected by the pandemic, and they’ve lost two or three years of development, in a time when we are all struggling to try and figure out what we’re doing next.”
The panelists believed that the pandemic contributed to relapses in recovery.
“I had patients that had long-term recovery that once COVID hit, it really induced anxiety and fear,” said Dr. Reyes-Walsh. “Then, you couple that with the isolation and then not being able to get to their recovery meetings and have the support of their network. It was pretty, pretty upsetting to see the amount of relapse that happened. … I had double digits losses of patients, which was traumatic for me to experience because these were patients that I had long-term relationships with – that had long-term recovery – were now lapsing in their recovery and then dying from their addiction.”
“When the isolation started and a lot of the COVID things came into play … we had a lot of people that just started day drinking and went from a few days a week to maybe on the weekends to really just every single day,” contributed Dr. Pannel. “We saw a huge increase in consumption of everything from food, drugs, alcohol, all of the above.”
GeneSight as part of the treatment plan
Dr. Pannel says his state, Mississippi, struggles with the number of patients needing treatment against a shortage of providers. That means that providers often have less time for repeat patients, which leaves less time for trial and error with mental health medications.
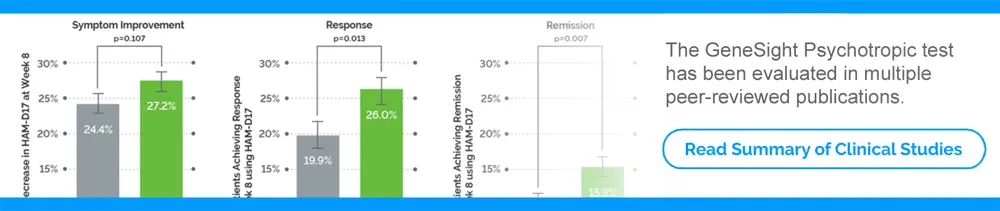
“When I talk to colleagues in the community and providers, a lot of times, they give it their best effort. They try to start people on medications. They try to do a pharmaceutical approach and people that deal with psychiatry medicines know that sometimes that cannot be as effective as you would like. There’s a lot of side effects potentially, or people can have a different reaction,” said Dr. Pannel. “…So the way we utilize the GeneSight [test], and thankfully have been in partnership with them for a long before this happened, was to do this and talk with patients, talk with families. Because even if there not been any medication trials already, when people are coming in off the street, chemicals, drugs, alcohol, other things, it’s important to be able to check and discuss with them and talk about a very specific, accurate approach for them and sort of to get out of the trial-and-error approach.”

Further, it helps him help patients better adhere to the medication regime he prescribes.
“The biggest thing that I use it for, that a lot of people don’t think about, is when we talk about it and we instill that confidence with patients and families, it really helps promote compliance with the medications,” said Dr. Pannel. “Anybody that prescribes psychiatric medications will tell you our biggest pitfall is either noncompliance from the beginning or noncompliance during the course of treatment when things have gotten a little bit better. But I find when we go back to that testing and utilize that real image of what we have is the information, it really instills a lot of confidence and compliance.”
“If there is any apprehension [about starting medications], whether it’s they haven’t been on meds in a long time, or they’ve never been on meds, or they have been on many different meds, I take all those reasons and say that is the reason why we need to do GeneSight. Because we can get a much better clinical picture of the way your body metabolizes medicine, so we can make the right choice, hopefully, the first time and get you started on something and get you feeling better right away, as opposed to putting off and starting with therapy first,” agreed Dr. Reyes-Walsh. “…Because it’s so hard to get in with a therapist.”
Primary care providers are on the front lines
Dr. Reyes-Walsh encourages primary care providers – who are on the front lines of diagnosing addiction and mental health issues – to conduct a comprehensive and deep assessment to determine if there are underlying addiction issues.
“If they do think that [there is] an addiction issue, they can certainly refer that patient to me,” said Dr. Reyes-Walsh. “But there are medications that they can prescribe that can help. I talk to primary care providers quite often and consult with them to help them through the process [of medication selection] so that they feel more comfortable.”
Dr. Pannel agreed: “It’s very empowering for any provider to have this tool [the GeneSight test] to work with if they need it.” He also noted that a lot of those in primary care and other healthcare specialties “didn’t really plan on addressing the large part of the mental health crisis that this country is in. But it shows up in their office every day.”
Johnson says that the GeneSight test has saved her time and lessened her stress.
“[The GeneSight test] is a time saver. It’s a stress saver. I mean it just makes life so much easier,” said Johnson. “Almost everybody [who] walks in your door is going to have at some point been put on an SSRI somewhere along the line, or a benzo for their anxiety… So, you have your means to just go ahead and pull that GeneSight… You’ll have that information for when that patient comes back. But it’s just to me, it’s a time saver, it’s stress saver, and it just does so much to help that patient relationship, to help that patient get relief.”
For more information on this topic and how GeneSight may help, visit:
To watch this GeneSight Cares webinar in its entirety, visit: https://genesight.com/genesight-cares/
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.