“I have this thing where I get older but just never wiser
Midnights become my afternoons
When my depression works the graveyard shift
All of the people I’ve ghosted stand there in the room
I should not be left to my own devices
They come with prices and vices
I end up in crisis (tale as old as time)”
– “Anti-Hero” by Taylor Swift
Depression and anxiety hit everyone differently, but many people felt the song “Anti-Hero” hit the nail on the head.
 “As someone who has dealt with a handful of mental illnesses for most of my life, ‘Anti-Hero’ (and its video counterpart) captures the complex feelings that often come along with deep self-loathing, body-image issues, and depression,” writes Jada Welch Olson on the PopSugar website. “…One of the worst characteristics of depression, or most mental illnesses for that matter, is how good they are at convincing you to isolate so they can grow stronger while guilt from abandoning the people you love stacks up.”
“As someone who has dealt with a handful of mental illnesses for most of my life, ‘Anti-Hero’ (and its video counterpart) captures the complex feelings that often come along with deep self-loathing, body-image issues, and depression,” writes Jada Welch Olson on the PopSugar website. “…One of the worst characteristics of depression, or most mental illnesses for that matter, is how good they are at convincing you to isolate so they can grow stronger while guilt from abandoning the people you love stacks up.”
If you love someone who has depression or anxiety, it can be hard to know how best to support them. After all, if you have never experienced a mental health condition, you may perceive a loved ones’ inability to get off the couch as slothfulness or being emotionally disconnected. You may grow frustrated with their seeming lack of desire to engage with you, their family or their friends.
“Well-intentioned people will say things like, ‘just think positive,’ or ‘just snap out of it.’ Though they may not say it out loud, some people think a person with depression is just being lazy, or just trying to get attention,” according to Richard W. Sears, PsyD, MBA, a board-certified clinical psychologist, in Greater Good Magazine. “However, major depressive disorder is a serious psychological condition.”
1. Learn the symptoms of depression and anxiety
The possible symptoms your loved one may show when experiencing depression or another mental illness like anxiety disorder can vary from person to person. According to the Mayo Clinic website, depression symptoms can include:
- “Feelings of sadness, tearfulness, emptiness or hopelessness.
- Angry outbursts, irritability or frustration, even over small matters.
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports.
- Sleeping too little or too much.
- Tiredness and lack of energy, so even small tasks take extra effort.
- Reduced appetite and weight loss or increased weight gain.
- Physical problems that can’t be explained, such as back pain or headaches.
- Anxiety, restlessness or nervousness.
- Slowed thinking, speaking or body movements.
- Feelings of worthlessness or guilt, focusing on past failures, or blaming yourself for things that aren’t your responsibility.
- Trouble thinking, concentrating, making decisions and remembering things.
- Frequent or repeated mention of not wanting to live, suicidal thoughts, suicide attempts or suicide.”
Seeing what these symptoms may look like in daily life can be helpful in understanding where your loved one is coming from. The “How Depression Feels” site offers a first-hand view of the world from the eyes of a person with depression and may offer you a sample of your loved one’s thoughts or feelings.
Likewise, anxiety is important to understand. Those who have generalized anxiety disorder can’t just “not worry about it.”
“Anxiety and worry are not the same thing. Worry is situational. Anxiety is persistent and excessive – and it doesn’t go away when the specific cause of stress or distress is gone,” said Debbie Thomas, EdD, APRN, based in Louisville, Ky shared in a GeneSight Mental Health Monitor news release. “Every day in my practice I see children and young adults and/or their parents who have unintentionally ignored or minimized the symptoms of anxiety until they become a crisis. The best outcomes occur when we don’t wait until anxiety becomes all-consuming and life-disrupting.”
According to the National Institute of Mental Health, generalize anxiety symptoms may include:
- “Feeling restless, wound-up, or on-edge
- Being easily fatigued
- Having difficulty concentrating
- Being irritable
- Having headaches, muscle aches, stomachaches, or unexplained pains
- Difficulty controlling feelings of worry
- Having sleep problems, such as difficulty falling or staying asleep”
If you see any of these kinds of symptoms in a loved one, the next step is communication.
2. Ask the person to open up about what they’re going through
If you’re worried about your loved one’s mental health, you may want to speak to them directly about what they are dealing with. On the Mayo Clinic website, the first step listed to help someone living with depression is to talk with them about your concerns.
“People with depression may not know or admit that they’re depressed. They may not be aware of the symptoms of depression, so they may think their feelings are normal,” according to the website. “People often feel ashamed about their depression, mistakenly believing they should be able to overcome it with willpower alone. But depression seldom gets better without treatment and may get worse.”
Some people who’ve experienced a mental health condition say it can be challenging to connect with their loved ones about their feelings.
Putri Surya writes in a story shared on the Anxiety & Depression Association of America (ADAA) website:
“My parents are practicing Muslims who believed my mental illness was just all in my head and if I was closer to God, it would all just go away. With them constantly telling me that at the age of 13, I had no idea how to even deal with these issues I had. I would read the Quran and pray as they suggested, but it just made me more angry at God because I felt like I wasn’t making any progress. I also felt immense pressure like I had to get better in order for my parents to be fulfilled in their faith. It was like I was a prisoner in my own thoughts and I wasn’t allowed to feel how I needed to feel.”
Friends encouraged Putri to share her concerns with her parents.
“After some blood, sweat and tears, my parents came to their senses and took me to a therapist that I ended up really enjoying. He helped me get down to the nitty gritty of my issues and made me feel so validated,” writes Surya. “…My therapist discussed with my parents the process in which would help me get better and that included me being on medication. Though with some hesitation, my parents ended up agreeing that that was the best plan for me.”
This situation is not unique. Parents may often struggle with identifying and talking about mental health challenges, but a GeneSight Mental Health Monitor found that “three in four young adults surveyed who have experienced a mental health challenge indicated at least some of their challenges occurred before age 18, yet half said their parents never sought treatment for them.
Nearly three quarters of these young adults wish that their parents would have. When asked why:
- 67% said they wouldn’t have suffered so much during their teenage years
- 66% said they would be better equipped to handle their current problems
- 64% said it would have better prepared them for adulthood”
If you are a loved one and worried that you aren’t supporting someone on their mental health journey, the Mental Health Association of America offers some valuable information and resources on its website. There is a downloadable worksheet that helps loved ones think through how have a conversation about mental health.
3. Look after yourself
When you’re helping support a loved one who is struggling, it’s important to also take care of your own mental health needs.
“Family members often experience a combination of burnout, guilt, psychological stress, and anxiety,” says Lena Suarez-Angelino, MSW, LCSW, a bilingual mental health therapist in a Verywell Family article. “After a while, it can become extremely difficult to watch a family member go through the ups and downs of depression.”
A PsychCentral article suggests that caregivers should look for ways to find joy in their lives. That may include developing friendships separate from a family dynamic. Further, it’s important to practice self-care – like exercising, eating well, trying to get a good night’s rest, and finding ways to relax.
Further, it’s important to not take it personally – which is easier said than done.
“Try to understand that the way your partner is acting isn’t intentional or personal. Their behavior isn’t about you at all,” according to the PsychCentral article. “It may be helpful to repeatedly tell yourself something along the lines of, ‘My spouse is having a tough time. They’re a good person, and they’re not intentionally trying to hurt me.’”
4. Talk to someone about what you’re dealing with
Connecting with others may also help. Sometimes, just having a family member or friend to vent to is enough to get you through a particularly stressful time. So, scheduling regular socializing time is important – whether that’s grabbing a cup of coffee, taking a walk or video chatting with a friend.
Yet, sometimes with even the most helpful and supportive family and friends, it’s not enough.
The Mayo Clinic suggests that you may want to try reaching out to professional organizations like caregiver associations or joining a support group.
“Many communities have classes specifically about the disease your loved one is facing. Caregiving services such as transportation, meal delivery or housekeeping may be available,” according to the Mayo Clinic website. “…A support group can provide validation and encouragement, as well as problem-solving strategies for difficult situations. People in support groups understand what you may be going through.”
5. Assist the person with depression and/or anxiety in getting help
Even if your loved one realizes they are struggling, they may need your help to move forward.
“Active depression is definitely something people need help moving through, because they lose their motivation. Sad feelings, negative perceptions, exhaustion, and withdrawal from activities lead to a downward spiral,” according to Dr. Sears in Greater Good Magazine. “…The best thing you can do is patiently but firmly encourage someone with depression to seek professional help. There are a wide variety of effective psychotherapy approaches for the treatment of depression. Encourage the person to look for someone they feel a connection with so that they will be motivated to stick with treatment. There are also a number of good medication options, so encourage the person to seek out a consultation with their primary care provider or a psychiatrist.”
It isn’t easy to watch a loved one deal with mental health issues, but you don’t have to go through this experience alone. Together, you can find help.
For more information, please read our other blog posts:
https://genesight.com/blog/patient/life-impacts-of-depression/
https://genesight.com/blog/patient/what-is-respite-care/
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
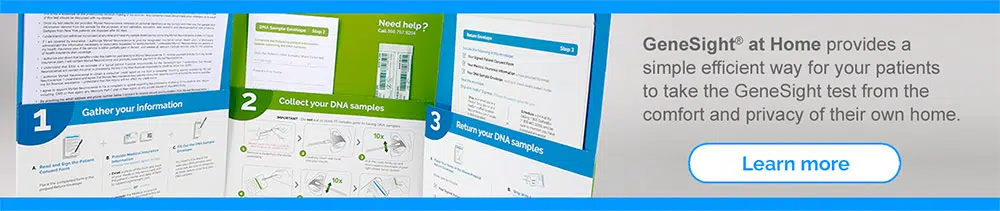
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.