Does your office voicemail include the message: “If this is an emergency, please hang up and call 911”?
If your patients do call 911, they often find themselves in an ambulance riding to visit the nearest emergency room (ER).
But ERs are often overtaxed and at capacity. In fact, more than 117 million patients were treated in ERs across the country last year – and patients spend three hours on average during their visits, according to the New York Times.
A number of these patients are entering the ER with psychiatric complaints – suicidal or violent thoughts, psychosis, substance-use disorders, and that number is increasing. Since 2006, ER visits for mental health disorders have increased more than 50 percent. According to the Agency for Healthcare Research and Quality, one in eight ER visits now involves a psychiatric emergency.
In addition, a recent study of about 3.5 million individuals published in the Journal of the American Medical Association shows that individuals with mental health diagnoses make 25 percent more visits to the emergency department (ED) than those without mental illness; increases in frequency correspond to illness severity.
Mental Health Emergency + Shortage of Psychiatrists = ER Crisis
But increasing ER visits for mental health reasons isn’t a cause – it’s a symptom of a much larger problem. There is a mental health emergency in America.
According to the National Institute of Mental Health, 16.2 million adults in the United States – 6.7 percent of all adults in the country – have experienced a major depressive episode in the past year. However, there are not enough practicing mental health professionals to help those suffering.
The need for psychiatric services is expected to rise as the number of psychiatrists falls. According to the Association of American Medical Colleges (AAMC)’s newsletter, AAMC News, the U.S. “is suffering from a dramatic shortage of psychiatrists and other mental health providers. And the shortfall is particularly dire in rural regions, many urban neighborhoods, and community mental health centers that often treat the most severe mental illnesses.”
Multiple factors contribute to the shortage. Psychiatrist and neuroscientist Dr. Darrell Kirch, CEO of the AAMC, told NPR recently: “The population is growing, and aging. The segment of the population growing the most are those over 65. They have the highest healthcare needs and that includes mental disorders.”
ER Visits for Psychiatric Emergencies

Scott Zeller, MD, vice president of acute psychiatry at Vituity, tells Health Leaders Magazine that the opioid epidemic, a significant increase in suicide attempts, and fewer inpatient psychiatric beds contribute to more behavioral health patients in hospital emergency departments.
In a column for STAT News, Dr. Anne Zink says the problem is also driven in part by “too few outpatient resources and inpatient treatment options for mental health issues; and separate systems for treating mental health and physical health.”
For many patients in crisis, the ER is the only option – and most ERs are not equipped to handle it. 84% of physicians report psych patients being “held” in the ER, according to a recent poll of emergency physicians by the American College of Emergency Physicians (ACEP).
According to Dr. Zink, “Part of the answer is the function of the emergency department in today’s healthcare system. I think of it as an overflow tank. When one part of the healthcare system fails, problems trickle down and come to rest in the emergency department. The tremendous fear and stigma associated with mental health makes the problem worse, as many patients fail to seek help at the onset of a mental health issue.”
Many stays in the emergency department can last for hours; some even stay for a few days when there are no psychiatric beds available. The practice, called psychiatric boarding, occurs largely because no appropriate mental healthcare is available.
Delivering psychiatric care in the ER is not easy. Most ER physicians are not trained to manage patients who present with suicidal thoughts, or have borderline personality disorder, or schizophrenia. For those patients, the ER environment – loud, bright, and with constant motion and stimulation – can exacerbate the psychiatric emergency that brought them there.
Increasing Psychiatric Care in the ER– and Out
Dr. Zeller says that they’ve already seen positive results: “In the units I have been involved with, less than 1% of patients need to be restrained compared to 50% in the regular ER. Patients also respond well to treatment, with 75% of EmPath Unit patients being discharged home or somewhere less restrictive, wherein typical models 100% might be hospitalized.”
ACEP proposes several solutions to better address the needs of patients with psychiatric issues who come to the emergency department. A few include:
- Increased hospital inpatient staffing and capacity. Additional psychiatric inpatient beds would help to alleviate boarding for those patients who require hospital-level care.
- Increased education. Provide additional training and education to ER personnel on psychiatric stabilization.
- Increased Outpatient Capacity/Community Alternatives. Two community services that have shown promise were crisis residential services and mobile crisis teams. Crisis residential settings could care for patients who do not need to be in a hospital setting, allowing the emergency department to see more acute medical patients. Mobile crisis, often referred to as diversion teams, provide crisis intervention and stabilization services to psychiatric patients in the community, preventing many patients from seeking care in the emergency department.
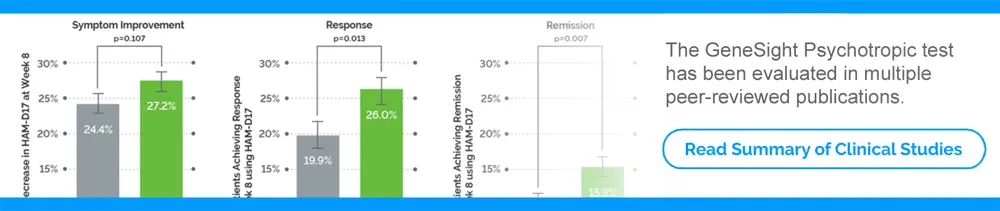
- Innovative Psychiatry (Tele-Psychiatry & Psychiatrists as Hospitalists). Use of tele-medicine would allow psychiatrists to perform evaluations and screenings of psychiatric patients when they cannot be physically present in the ER. This would allow for early medication intervention and could alleviate inappropriate inpatient admission, leading to reduced boarding. Some companies are even introducing ways to conduct testing historically administered in an office setting. For example, clinicians registered with GeneSight can use GeneSight® at Home to send patients an easy-to-follow sample collection kit.
There is clearly no shortage of ideas. What is the best way to implement them efficiently – and effectively?