Thousands of mental health care workers at Kaiser Health facilities in northern California went on strike in the summer of 2022. They say that Kaiser is not complying with a California law that requires health plans to make follow-up appointments for mental health patients in a timely manner, according to a story on KQED. They are demanding the healthcare system increase mental health staffing and wages.*
Kaiser Permanente’s regional senior vice president of human resources responded in a statement that while they have “the deepest appreciation and gratitude for our mental health professionals and the extraordinary care they provide to our members…there are not enough mental health care professionals to meet the increased demand for care.”
This is hardly stonewalling by Kaiser. This shortage certainly existed before the COVID-19 pandemic. However, in the past few years, demand for mental health services has skyrocketed. The number of adults reporting symptoms of depression and anxiety has nearly quadrupled during the pandemic.
Yet, little has been done to address both the increase in patients and the shortage of mental health professionals.
Why is there such a shortage of mental health professionals?

The reasons for the shortage are many – an aging workforce, physician burnout, lack of psychiatric residency spots, lack of insurance coverage and reimbursement, failure to recruit new professionals to the industry. Solving the problem will require a variety of tactics, both creative and practical.
Robin M. Johnson, MD, wrote in a commentary published in the Psychiatric Times:
“Clearly it is essential to have more psychiatrists, but how do we increase the psychiatry workforce to reach all the shortage areas in the country? Although the description of the shortage is clear, the solutions to the problem have not been. Without an intervention, the shortage is projected to continue until 2050.”
“We’re not taking new clients at this time”
Those looking for help with their mental health today are running into a brick wall of clinicians having full panels – and selective insurance acceptance with those who are taking new patients.

“I have been looking for a therapist for years now sporadically, and in earnest for the past few weeks,” Bodie P. (not his real name), a GeneSight patient. “Even when I find someone who is taking new patients, many don’t take my (or any) insurance. And if you want to see them in person it narrows the field even further. It is so frustrating that it has actually made my depression and anxiety worse.”
According to a recent Chicago Tribune article, “Many mental health professionals no longer take health insurance because they say they’ve grown frustrated with insurance companies not paying them enough, taking too long to pay and making them jump through hoops to give patients the care they need.”
On the other side of the equation, healthcare workers may be suffering burnout, as working with mental health patients may take a toll.
“The job is really, really hard,” says Eric Morse, CEO, The Centers in Cleveland, a nonprofit that offers counseling and psychiatric services. “The caseload should be around 40 to 50 because these are people who need a lot of attention. Because of the staffing shortage, caseloads being at 100, it really changes the work. It changes your ability to respond to the needs of everyone you’re serving.”
Increased pressure on PCPs to provide mental health services
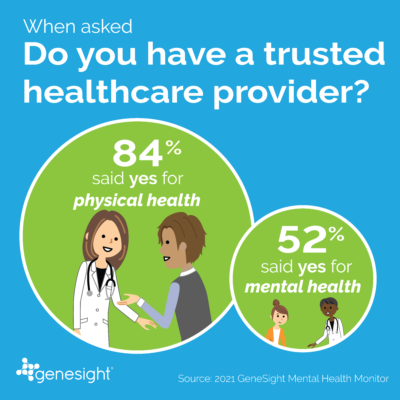
This leaves Primary Care Providers (PCPs) on the frontlines of the crisis. In fact, a study found that nearly 60% of patients who receive mental health treatment do so from their PCP. Yet, a 2022 GeneSight® Mental Health Monitor found that fewer than 25% of patients were given a depression screening at their primary care appointments.
Further, a 2021 GeneSight Mental Health Monitor found that two out of three of respondents said annual doctor visits are one of the best ways to take care of physical health, but only one out of three said that approach was good for mental health. Nearly half of respondents in the 2021 survey (46%) said primary care physicians would be the first healthcare provider they would talk to about their mental health concerns. Next would be a therapist/counselor (29%).
“Screening for depression is important because depression is one of the leading comorbidities of debilitating physical health conditions such as diabetes,” Dr. Charles Cook, a family nurse practitioner in Winston-Salem, N.C., said in a recent GeneSight Cares webinar. “It can be difficult to treat chronic diseases without also addressing co-morbid depression. Depression screening improves our ability to diagnose and treat our patients, and it saves time for the clinician, the patient and for other providers.”
PGx may help PCPs
Pharmacogenomics (PGx) testing, such as the GeneSight test, may be one tool to help PCPs manage their patients’ mental health. The GeneSight Psychotropic test analyzes clinically important genetic variations which may impact how a patient metabolizes and responds to certain FDA-approved medications used in the treatment of depression, anxiety, ADHD and other mental health conditions. The GeneSight Psychotropic report provides clinicians with information about which medications may require dose adjustments, be less likely to work, or have an increased risk of side effects based on your patient’s genetic information. The test is intended to supplement other information considered by a clinician as part of a comprehensive medical evaluation.
“For a primary care doctor… to do a GeneSight test really would cut down on some of the referrals I even get from the start,” said Dr. Crystal Nelson, a psychiatrist in Newnan, Ga, during a recent GeneSight Cares webinar ‘Are You Playing Offense or Defense with Your Patients’ Mental Health.’ “If a medication choice is made with as much information as the GeneSight report gives, patients might get better outcomes.”
*UPDATE:
After this blog was posted, MedCityNews reported “Kaiser Nurses Ratify New Contract That Raises Wages by 22.5% And Improves Staffing.”
For more information about this topic, please visit:
The Importance of Screening for Depression in Primary Care https://genesight.com/blog/healthcare-provider/the-silent-illness-the-importance-of-screening-for-depression-in-primary-care/
Am I a Good Candidate for GeneSight Testing? https://genesight.com/genetic-insights/am-i-a-good-candidate-for-genesight-testing/
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.