A faster route to medication insights
What is the GeneSight® Test?
The GeneSight Psychotropic test is designed to analyze clinically important genetic variations that may impact how your patients metabolize and respond to certain mental health medications. These pharmacogenetic insights can provide critical information to inform treatment plans and may help shorten your patients’ road to wellness.

Backed by extensive research
7 clinical studies published in peer-reviewed journals support the GeneSight test’s effectiveness.
GUIDED clinical study
The largest patient and rater blinded pharmacogenomic study in mental health.1
Key findings
The GeneSight test outperformed treatment as usual.
relative improvement in depressive symptoms2
relative improvement in response rates3
relative improvement in remission rates4
Get started with easy ordering and complimentary report consults
Fill out this form and a GeneSight representative will contact you to complete the registration process so you can begin offering the GeneSight test to your patients.
Once registered, place an order on mygenesight.com
Your practice collects your patient’s DNA sample with a simple cheek swab OR your patient uses the home collection kit.
The DNA sample is sent to our lab for analysis. After the sample is received, the GeneSight report is typically available in 2 days.
Use the genetic insights from the GeneSight report to help inform your treatment. Contact our medical team for a complimentary report interpretation consultation.
Genetic insights to help navigate your patient’s next treatment
The GeneSight Psychotropic report may help you avoid multiple medication trials by providing information about which medications may require dose adjustments, be less likely to work, or have an increased risk of side effects based on your patient’s genetic information.
The report also includes information on how a patient’s smoking status may affect their body’s metabolism of certain medications.
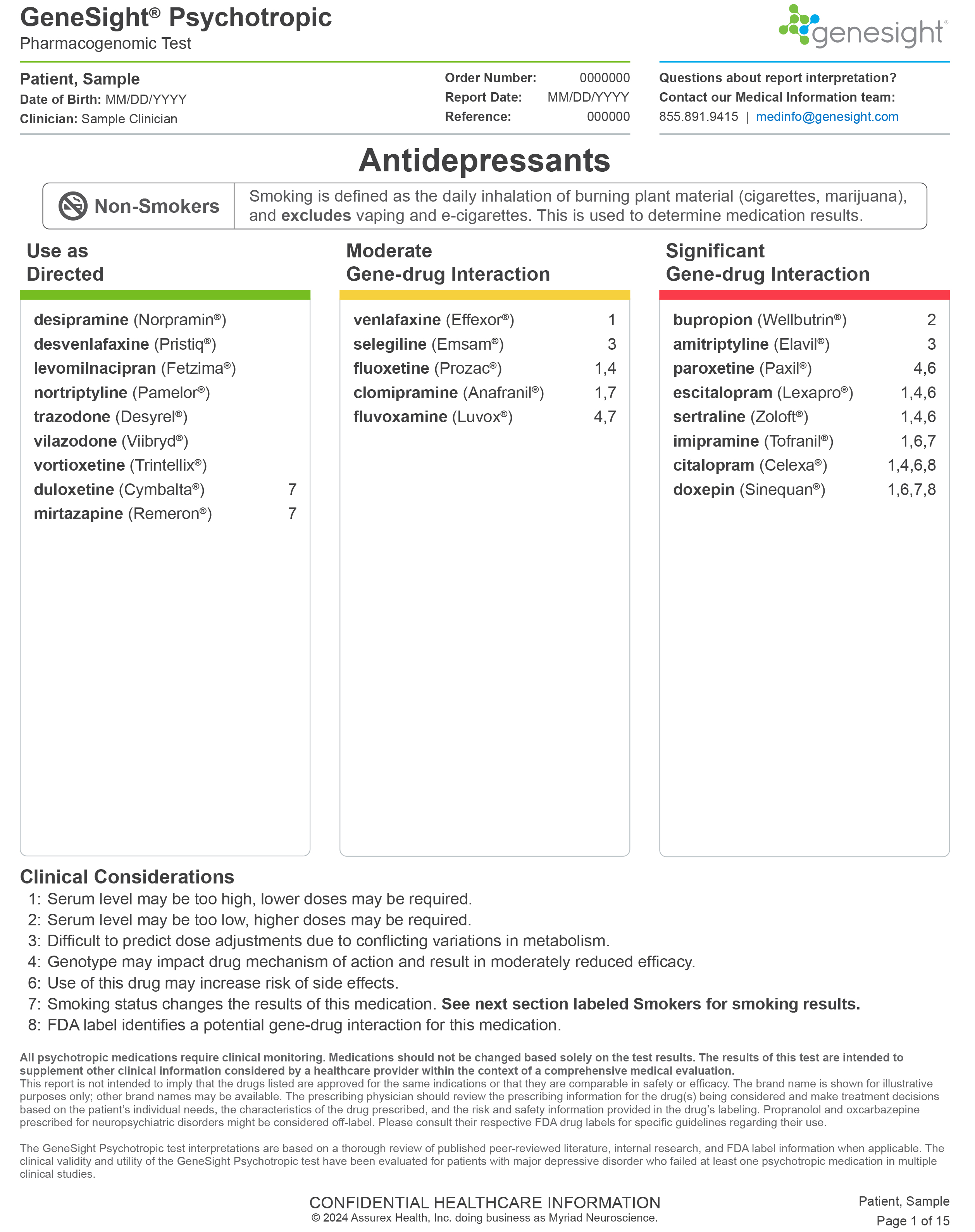
- Use as directed
- Moderate gene-drug interaction
- Significant gene-drug interaction
The report classifies over 60 mental health medications into three categories.
The GeneSight test results do not provide information on disease diagnosis, medication allergies, drug-drug interactions, or which medications will work best.

Get insights for many types of mental health patients and medication histories
An ideal time to consider the GeneSight test is when treating:
- New patients with a previous medication failure
- Patients experiencing lower-than-desired medication response
- Patients experiencing unwanted side effects
- Elderly patients
- Patients with liver damage

We’re committed to helping your patients navigate cost
Our goal is to make the GeneSight test affordable and accessible to patients. Insurance can be complicated, and we want you to feel comfortable ordering the test for your patients.
Cost shouldn’t be a barrier to getting critical insights for informing mental health treatment.
And if your patient’s cost is estimated to be more than $330, we’ll contact your patient to discuss their options, including financial assistance and interest-free payment plans for those who qualify.
* Based on a review of six months of past claim data for major insurance carriers across the US. Last updated 2023.
7 clinical studies
Go forward with the GeneSight Test: the only pharmacogenomic test evaluated in 7 clinical studies published in peer-reviewed journals.
Clinician resources
Hear from other healthcare providers
Tens of thousands of clinicians have ordered the GeneSight test for 3 million patients and counting. Explore what happens when the GeneSight test becomes part of a clinician’s practice through the testimonials shared below.
The stories shared on this page are individual healthcare providers’ personal experiences with GeneSight. Others may not have the same experience or outcome. Do not make any changes to your current medications or dosing without consulting your healthcare provider.

References: 1. Jablonski MR, King N, Wang Y, et al. Analytical validation of a psychiatric pharmacogenomic test. Personalized Medicine. 2018;15(3):189-197. doi:https://doi.org/10.2217/pme-2017-0094. 2. Shelton RC, Parikh SV, Law RA, et al. Combinatorial Pharmacogenomic Algorithm is Predictive of Citalopram and Escitalopram Metabolism in Patients with Major Depressive Disorder. Psychiatry Research. 2020;290:113017. doi:https://doi.org/10.1016/j.psychres.2020.113017. 3. Parikh SV, Law RA, Hain DT, et al. Combinatorial pharmacogenomic algorithm is predictive of sertraline metabolism in patients with major depressive disorder. Psychiatry Research. 2022;308:114354. doi:https://doi.org/10.1016/j.psychres.2021.114354. 4. Rothschild AJ, Parikh SV, Hain D, et al. Clinical validation of combinatorial pharmacogenomic testing and single-gene guidelines in predicting psychotropic medication blood levels and clinical outcomes in patients with depression. Psychiatry Research. 2021;296:113649. doi:https://doi.org/10.1016/j.psychres.2020.113649. 5. Winner JG, Carhart JM, Altar CA, et al. Combinatorial pharmacogenomic guidance for psychiatric medications reduces overall pharmacy costs in a 1 year prospective evaluation. Current Medical Research and Opinion. 2015;31(9):1633-1643. doi:https://doi.org/10.1185/03007995.2015.1063483. 6. Oslin DW, Lynch KG, Shih MC, et al. Effect of Pharmacogenomic Testing for Drug-Gene Interactions on Medication Selection and Remission of Symptoms in Major Depressive Disorder: The PRIME Care Randomized Clinical Trial. JAMA. 2022;328(2):151-161. doi:https://doi.org/10.1001/jama.2022.9805. 7. Greden JF, Parikh SV, Rothschild AJ, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: A large, patient- and rater-blinded, randomized, controlled study. Journal of Psychiatric Research. 2019;111:59-67. doi:https://doi.org/10.1016/j.jpsychires.2019.01.003.