As the COVID-19 pandemic continues, depression and anxiety are on the rise. As a result, mental healthcare providers are being pushed to provide care to more patients, while keeping themselves, their staff, and patients safe.
Many are turning to telehealth as a way to provide treatment to patients when they can’t be seen in person. The integration of telehealth into traditional medicine could reach far beyond the pandemic and into the future.
Telehealth does have its positives and negatives, though. When implementing a plan for seniors and telehealth, healthcare providers should consider both the barriers and opportunities to conduct the most effective telehealth visits for their patients and themselves.
Are Mental Telehealth Visits as Effective as In-Office Mental Health Visits?
Yes, they can be. According to an article published in Annual Review of Clinical Psychiatry, evidence from more than 100 controlled trials suggests that guided Internet treatments for a wide range of psychiatric and somatic conditions “can be as effective as face-to-face treatments, lead to sustained improvements, work in clinically representative conditions, and probably are cost-effective.”
The Commonwealth Fund concurs in its To the Point blog post, stating “numerous studies have demonstrated [telehealth’s] effectiveness across a range of modalities (e.g., telephone, videoconference) and mental health concerns (e.g., depression, substance use disorders). Virtual services are safe, effective and comparable in outcomes to in-person services.”
Mental Healthcare Providers, Older Adults, and Telehealth Usage
“Video-based telepsychiatry helps meet patients’ needs for convenient, affordable, and readily accessible mental health services,” according to the APA.
According to the 2020 Survey of America’s Physicians, conducted by Merritt Hawkins in collaboration with The Physicians Foundation, 48 percent of U.S. physicians currently are treating patients through telemedicine compared to only 18 percent in 2018.
Meanwhile, 26 percent of people 50 to 80 years old reported having had a virtual medical visit since the outbreak of COVID-19, according to the University of Michigan (U of M) 2020 National Poll on Healthy Aging (NPHA). This is compared to only four percent in the 2019 NPHA.
Why is Mental Telehealth Important for Older Patients?
There are multiple, potential benefits for older adults who use telehealth to communicate with their mental health practitioners.
At the top of the list is access, according to the APA. During the pandemic, access is vital, especially since some seniors may be immunocompromised. Additionally, bringing care to the patient’s home or location via telehealth may open possibilities for those who live in remote or rural areas to connect more easily with mental healthcare specialists.
The APA suggests several other benefits of telehealth including:
- “Help integrate behavioral health care and primary care, leading to better outcomes
- Reduce the need for trips to the emergency room
- Reduce delays in care
- Improve continuity of care and follow-up
- Reduce the need for time off work, childcare services, etc. to access appointments far away
- Reduce potential transportation barriers, such as lack of transportation or the need for long drives
- Reduce the barrier of stigma”
Telehealth becomes especially important as more older adults are suffering from mental disorders at a time when their ability to meet with healthcare providers in person has decreased significantly.
Statistics from the American Association for Geriatric Psychiatry show that 20 percent of adults age 55 and older have a mental health disorder such as anxiety, cognitive impairment, or mood disorder. More recent data from the Centers for Disease Control and Prevention (CDC), gathered between April and August 2020, show that week by week, the number of adults aged 50 to 59 who reported suffering from either depression or anxiety has risen to levels as high as 40 percent. Additionally, those in the 60 to 69 age range showed highs of 32%, while those in the 70 to 79 or the 80 years and above age ranges showed highs near 25%.
Geriatrician Laurence M. Solberg, MD, who has been using telemedicine through the U.S. Department of Veterans Affairs (VA) for more than a decade, writes in the Institute for the Healthcare Improvement blog that “televisits are especially good for frail, older people because they don’t get worn out from the traveling to your office.”
Solberg recognizes that in spite of the benefits, there are communication challenges that practitioners may need to manage when using telehealth with older patients. Particularly, some providers may find it hard to make sure that communication with older adults over an audio line or video screen does not seem impersonal or give the impression that the provider is “just going through the motions.”
To overcome these obstacles, he recommends that providers consider using the 4Ms Framework:
- Address what MATTERS to the patient in terms of their goals, preferences and priorities
- What MEDICATIONS they currently take
- Their level of cognitive impairment or MENTATION
- Their level of MOBILITY
“Using the 4Ms Framework is a simple way to personalize telemedicine and make it more supportive of older patients,” Solberg writes.
How to Make Telehealth Easier for Older Patients
While older adults in the 2020 U of M poll expressed that they were increasingly comfortable with telehealth (64 percent of older adults in 2020 felt very or somewhat comfortable with video conferencing technologies, up from 53 percent in 2019), “not all older adults see virtual care as an adequate substitute for in-person care, even in a pandemic.”
The APA Committee on Aging writes that providers may need to overcome some limitations in order to provide effective remote mental healthcare for older adults. The APA advises that providers consider the following:
- “Sensory and motor changes.” Due to some age-related sensory and motor changes, patients may need guidance regarding the home environment in which to set up their telehealth visit. Providers should encourage the patient, if needed, to get help setting up an environment where lighting and noise do not become distractions. Additionally, it is important that those who have issues with muscle strength or tone have a comfortable place from which they can access the telehealth technology.
- “Cognitive changes.” Most older adults experience some cognitive changes, but this should not prevent the use of telehealth. If the patient has cognitive challenges, a family member or other support person may need to set up the patient’s account and/or help them use the technology to communicate.
- “Strategies for establishing rapport.” The first telehealth appointment a patient does is likely to have some awkwardness as patients adjust to the technology and new experience of seeing their provider over a screen rather than in person. Accordingly, providers could look for new ways to establish rapport. Some ways to do this are to look directly at the camera, to reflect the patient’s language, and to verbally clarify ambiguous language and body language.
- “Strategies for providing technology support.” In terms of understanding the technology, healthcare providers should clarify the patient’s comfort level with the platform and clearly explain how to set up the technology and what to expect from the start to the end of the telehealth session.
Additional Strategies to Provide Technology Support for Older Patients
According to the APA Committee on Aging, when using telehealth with older adults, healthcare providers should not assume discomfort with either technology or the specific platform being used. They should assess the patient’s comfort level and with that in mind, provide technology support according to their needs and the following APA suggestions for things to do prior to the first appointment:
- Call (or have your staff call) the patient to provide verbal instructions, test the platform, and ensure the patient knows how to use the technology.
- Provide clear, written instructions in an easy-to-read format, including screen shots of the steps.
- Advise the patient, either verbally or in written form, on ways to enhance the ability to use the technology. For example, the patient could raise the display illumination, adjust the volume settings, use closed captioning, and keep the video platform clear of background visuals or noise.
The APA suggests that healthcare providers should provide the patient a summary of what needs to be completed before their next telehealth visit.
How Mental Healthcare Providers Can Manage Telehealth Restrictions
Although telemedicine practices have been around for years, “widespread implementation has been constrained by laws, regulations, and policies at national, state, and organizational levels. Federal and commercial payers have not covered many of these services,” according to an editorial in the journal Neurology.
Some of those restrictions have been lifted, a silver lining to the current COVID-19 health crisis. For example, Medicare coverage has been expanded for telehealth.
In all likelihood, telehealth is here to stay. For healthcare providers looking to build your telehealth capacity, it’s important to stay informed about changing laws and regulations, adapt workflows and staffing functions, and develop effective telehealth models.
Those models should be “built on a strong, reliable infrastructure, with the ability to scale, and become embedded within normal operations after the crisis resolves,” according to the editorial in Neurology.
The Future of Telehealth for Mental Healthcare Providers
As healthcare providers review ways to implement telehealth, they may find there is a lot of new material to digest, but there also are guides and resources to help along the way.
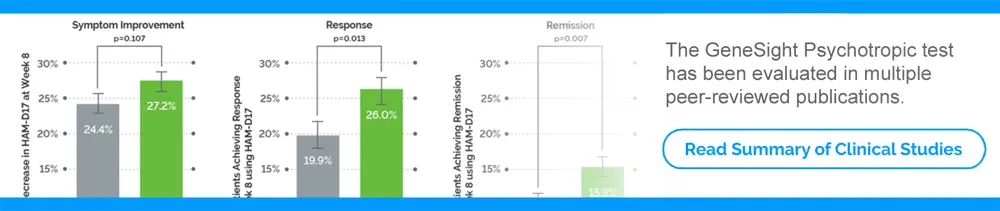
To help patients staying home, some companies are introducing ways to test at home that usually must be completed in a doctor’s office. For example, healthcare providers can now order the GeneSight test using GeneSight® at Home, allowing patients to collect and send their GeneSight test through an at-home patient collection kit. View instructions for ordering GeneSight at Home.
To learn more about seniors and mental health, please read:
Our articles are for informational purposes only and are reviewed by our Medical Information team, which includes PharmDs, MDs, and PhDs. Do not make any changes to your current medications or dosing without consulting your healthcare provider.
The GeneSight test must be ordered by and used only in consultation with a healthcare provider who can prescribe medications. As with all genetic tests, the GeneSight test results have limitations and do not constitute medical advice. The test results are designed to be just one part of a larger, complete patient assessment, which would include proper diagnosis and consideration of your medical history, other medications you may be taking, your family history, and other factors.
If you are a healthcare provider and interested in learning more about the GeneSight test, please contact us at 855.891.9415. If you are a patient, please talk with your doctor to see if the GeneSight test may be helpful.